“Robust evidence shows that diabetes is preventable through lifestyle modifications aiming at weight loss. A meta-analysis including 19 randomized clinical trials confirmed the long-term beneficial effect of lifestyle interventions, even with modest weight loss. Most of these interventions targeted weight loss through an energy-reduced, healthy low-fat diet combined with increased physical activity. However, no previous trial has assessed the effect of energy reduction in the context of a relatively high-fat diet, such as the Mediterranean diet (MedDiet).
The PREDIMED (Prevención con Dieta Mediterránea) trial demonstrated that an ad libitum MedDiet supplemented with either extra-virgin olive oil or mixed nuts reduced diabetes incidence by 30%, compared with a low-fat diet. However, this reduction occurred with only marginally reduced body weight. Building on this finding, the PREDIMED-Plus trial was designed to test whether adding caloric restriction and physical activity to the MedDiet would provide additional benefit beyond the effect observed only with the MedDiet. In a 1-year interim analysis, an energy-reduced MedDiet (erMedDiet) combined with increased physical activity significantly reduced body weight, waist circumference, and other cardiometabolic risk markers compared with an ad libitum MedDiet. The present analysis, conducted with data from all PREDIMED-Plus participants free of diabetes at baseline, tests whether an intensive lifestyle intervention aiming at weight loss reduces diabetes risk beyond the effects of an ad libitum MedDiet.
Methods
[..] Eligible participants were community-dwelling men aged 55 to 75 years and women aged 60 to 75 years, with overweight or obesity (body mass index [BMI] ≥27 and <40 kg/m2), without documented cardiovascular disease or diabetes (for the present analysis), and with at least 3 metabolic syndrome components: waist circumference 80 cm or more in women and 94 cm or more in men, elevated triglycerides (≥1.69 mmol/L [≥150 mg/dL]), a reduced high-density lipoprotein cholesterol level (<1.04 mmol/L [<40 mg/dL]), elevated blood pressure (systolic ≥150 and diastolic ≥85 mm Hg), and an elevated fasting glucose level (≥5.55 mmol/L [≥100 mg/dL]). [..]
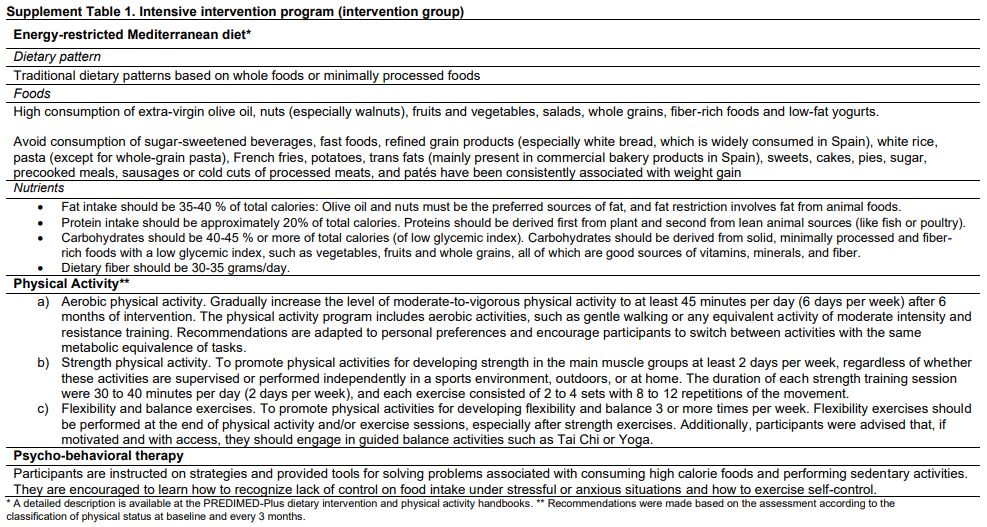
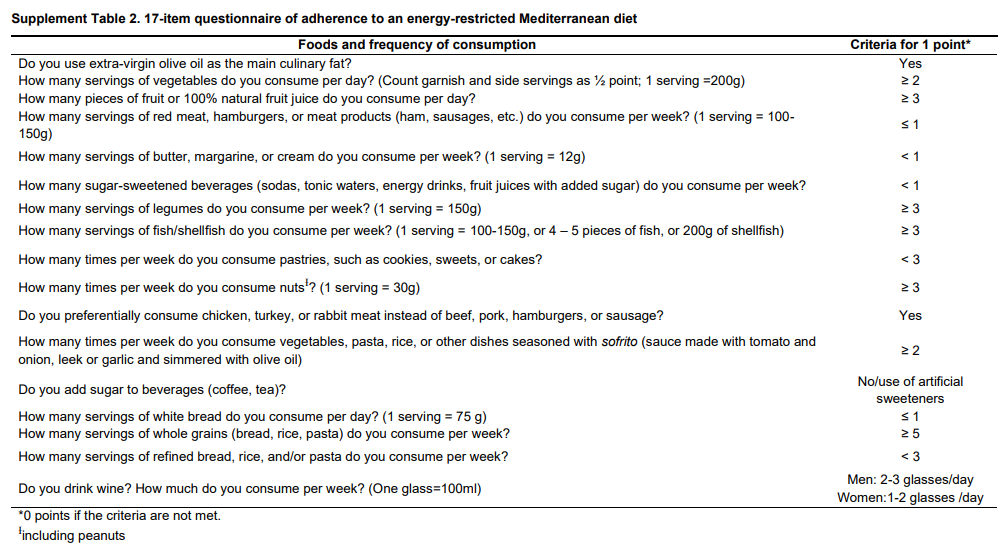
The erMedDiet was defined as a traditional MedDiet with a planned reduction of 600 kcal per day, providing 35% to 40% of calories from fat, 40% to 45% from carbohydrates, and approximately 20% from protein. Participants were encouraged to consume more fruits, vegetables, whole cereals, legumes, nuts, and extra-virgin olive oil, while limiting meat, sugar-sweetened beverages, foods with added sugars, and cream. [..] Physical activity recommendations included: a) progressively increased aerobic physical activity, mainly brisk walking, aiming for 45 minutes per day (or the equivalent) 6 days per week; b) strength exercises (≥2 days per week); and c) flexibility and balance exercises (≥3 days per week).
The control group received educational sessions on the traditional MedDiet with ad libitum caloric intake following the PREDIMED-1 trial recommendations. [..]
The participants in the intervention group were contacted by dietitians 3 times a month (1 group session, 1 individual session, and 1 phone call) during the first year, then received monthly group sessions, individual sessions every 3 months, and 2 phone calls every 3 months. Control group participants had 1 individual visit, 1 phone call, and 1 group session every 6 months. Both groups received 1 L per month of extra-virgin olive oil to support adherence and retention. [..]
Results
[..] After 6 years, the adjusted absolute risk difference for incident diabetes between the intervention and control groups was −2.4% (95% CI, −3.1 to −1.8), corresponding to a 31% (CI, 18% to 41%) relative risk reduction in the intervention group as compared with the control group.
In prespecified subgroup analyses, no statistically significant interactions were found for age, educational level, BMI, waist-to-height ratio, or baseline glucose level, except for sex, with greater diabetes risk reduction in men than in women (P for interaction = 0.035). [..]
Both groups showed similar increased use of antihypertensive and hypolipidemic medication. Participants in the control group had greater antidiabetic drug use than those in the intervention group during the follow-up (11.7% vs. 9.5% at year 6; P = 0.018).
[..] In the analysis of completers, the 6-year mean body weight reduction was −3.3 kg (CI, −3.4 to –3.1 kg) in the intervention group and −0.6 kg (CI, −0.7 to −0.4 kg) in the control group, representing weight reductions of 3.7% in intervention and 0.6% in control. During this period, mean waist circumference was reduced by −3.6 cm (CI, −3.8 to −3.3 cm) in the intervention group and −0.3 cm (CI, −0.4 to −0.1 cm) in the control group.
Discussion
[..] The MedDiet, rich in fiber, whole grains, antioxidants, and anti-inflammatory compounds, is known to reduce diabetes risk, even in the absence of weight loss. The erMedDiet fosters low glycemic index foods as well as more fiber and whole grains, which are known to improve insulin sensitivity. In addition, moderate physical exercise may protect mitochondrial function and protect against obesity-induced insulin resistance. Synergistically, reductions in weight and visceral fat, achieved through caloric reduction and the increased physical activity implemented in our intervention, could significantly lower insulin resistance and inflammation. The MedDiet and physical activity also trigger the secretion of incretin hormones such as glucagon-like peptide-1, which plays a crucial role in glucose metabolism. Finally, the intervention effect could be modulated by favorable changes in gut microbiota and metabolome. However, in our study, we cannot disentangle whether the greater reduction in diabetes incidence resulted from weight loss, enhanced adherence to the MedDiet, physical activity promotion, or any combination of their effects.
[..] The Diabetes Prevention Program (DPP) reported that an intensive lifestyle intervention, including a low-fat diet and enhanced physical activity, led to a 58% reduction in diabetes incidence compared with placebo over a mean follow-up of 2.8 years among persons with impaired glucose tolerance. Similarly, the Diabetes Prevention Study (DPS) reported comparable results after 3.2 years, also including patients with impaired glucose tolerance. More recently, 15-year follow-up of the DPP reported a 27% (CI, 17% to 35%) relative reduction in diabetes risk after lifestyle sessions were extended to all participants.
[..] The DPP trial achieved an average weight loss in the lifestyle intervention group of 5.6 kg (a 7% reduction of initial body weight), whereas the DPS trial saw 5% weight loss. In PREDIMED-Plus, 3.7% body weight loss over a period of 6 years was associated with long-term diabetes risk reduction. Therefore, even modest weight losses can lead to reductions in diabetes risk, consistent with previous studies. The potential effect modification by sex may be explained by greater weight losses in men (3.4 kg) than in women (2.3 kg), which was also observed in the DPP trial. However, these subgroup findings should be interpreted cautiously considering the number of comparisons performed.”
Full article, M Ruiz-Canela, D Corella, MA Martinez-Gonzalez et al. Annals of Internal Medicine, 2025.8.26
Accompanying editorial:
“The MedDiet focuses on high intake of plant-based foods; moderate consumption of fish, poultry, and dairy (along with optional red wine); and low intake of red meats, sweets, and sugar-sweetened beverages. Key components include extra-virgin olive oil, fruits, vegetables, legumes, nuts, and whole grains, which are known for their high-fiber, anti-inflammatory, and antioxidant properties, the mechanisms by which the MedDiet is presumed to decrease CVD risk. [..]
After 6 years, the adjusted absolute risk difference for incident diabetes between the erMedDiet intervention and the ad libitum MedDiet control group was −2.4% (95% CI, −3.1% to −1.8%), corresponding to a 31% (CI, 18% to 41%) relative risk reduction in the intervention group compared with the control group. Of note, a greater effect was observed in men compared with women. Although the seminal Diabetes Prevention Program (DPP) reported greater reductions in absolute (−14.4%) and relative (58%) risks for incident diabetes from a low-fat diet with physical activity compared with placebo for 3 years, PREDIMED-Plus’s longer duration of follow-up, use of a strong comparator (an ad libitum MedDiet), and older mean age of participants may in part explain the effect size differences. Weight loss was also greater in DPP than in PREDIMED-Plus, 7% versus 3.7%, respectively. This smaller reduction in weight, however, provides further evidence to clinicians and patients alike that even smaller reductions in body weight can lead to meaningful reductions in diabetes incidence.
[..] The study by Ruiz-Canela and colleagues shows us that diet quality is still important to consider and adds to the large body of literature demonstrating the important role that dietary intake and lifestyle modification can play in chronic disease prevention. Ultimately, this study contributes to the strong evidence base in support of the MedDiet as an optimal dietary pattern for long-term health.”
Full editorial, SJ Herring and GL Tripicchio. Annals of Internal Medicine, 2025.8.26