“Public health is an organized effort to protect and improve the health of populations through education, policy, and preventive programs (Table). Within public health, the concept of primordial prevention is well-defined as population-level efforts to prevent risk factors for incident or worsening disease, such as water sanitation systems. Primordial care is the individual-level equivalent: a person’s efforts to prevent the onset or worsening of sickness for himself or herself. This cognitive framing is a crucial distinction; individuals engaging in primordial care do not necessarily see themselves as sick or requiring treatment that would compel entry into the medical system. Individuals engaging in primordial care see themselves as needing nonmedical interventions to get healthy or healthier. Primordial care is not a formal public health program universally applied to everyone. It is heterogeneous, experienced differently by each person, and has been invisible to the public health system.
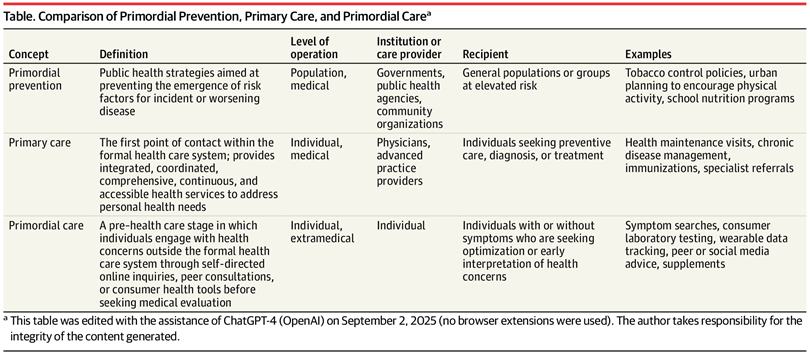
[..] Primary care is “the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community.” Primary care is an individual’s first point of contact within the health care system, typically with a physician, nurse practitioner, or physician assistant who delivers comprehensive, continuous care and coordinates treatment across specialties.
Primordial care is the pre–health care space where a person, who may be healthy or ill, is actively engaging with their health by researching symptoms on artificial intelligence search engines, consulting online forums and social media, purchasing over-the-counter remedies, and cross-checking their discovered information with friends and family. With current technology, primordial care is far from primitive, but it does feel primal, compelling individuals to explore instinctually and close to nature. Some individuals are healthy and are looking to preserve or optimize well-being. Others have early symptoms and are seeking reassurance or a nudge to enter the formal health care system, typically through primary care.
Although primary care is organized around the primary care physician, primordial care is intensely centered on the person. A person takes on all the risks and benefits of their beliefs, takes action or does not take action, and is the sole decision-maker. However, the boundary between primordial and primary care is porous. Some people pass through primordial care quickly on their way to establishing care with a primary care physician. Others remain in primordial care for years, cycling through online self-diagnosis, self-management, and peer advice without ever entering the health care system. The reasons for this lack of engagement are unknown but may be due to choice, cost, or stigma.
The primordial care the individual receives is likely dominated by the wellness industry, a parallel ecosystem that sometimes seems to substitute for, rather than complement, medical care. Wellness offerings can be empowering because they are accessible, consumer friendly, and often focus on prevention, lifestyle, and self-awareness. However, wellness offerings also carry the risk of misinformation, delayed diagnosis, unnecessary expense, and the illusion of safety if serious illness is present. Furthermore, the wellness industry is rarely held accountable due to minimal oversight and lack of requirements to prove health outcomes. The direct-to-consumer market, enhanced by telehealth, has blurred the transition and distinction between primordial care and medical care.
[..] Acknowledgment of this period in a person’s health journey is meeting patients where they are. Studying it would enable public health institutions to optimize an individual’s health literacy and agency, implement appropriate safety rails, and facilitate timely transitions into medical care while still preserving autonomy and accessibility. If the medical professional fails to recognize and respond, individuals are left with market forces and algorithms to shape the earliest interactions regarding their health. Ignoring primordial care creates a vacuum where patients can be misguided by social pressures, marketing, or financial incentives. With primary care rapidly losing its characteristic accessible-to-all banner, the consequence of allowing primordial care to remain unacknowledged and unaccountable is exactly the multidisease epidemic occurring today.
Research in the complementary and alternative medicine field, which may be part of primordial care or medical care, offers incomplete data. An estimated 23 000 emergency department visits per year have been attributed to adverse events due to dietary supplements3; however, the study was not designed to compare outcomes with pharmaceuticals approved by the US Food and Drug Administration. Further research is needed to understand the potential direct and indirect costs of primordial care (ie, resource overutilization, medical mistrust), the potential direct and indirect benefits (ie, increased engagement, high-risk innovation), and the comparisons with medical care.
In an era when health care access is disparate and trust in institutions is fragile, primordial care is where many health journeys begin and deserves the attention of our public health and medical communities.”
Full editorial, BG Tchang, JAMA, 2025.10.6