“In the United States, Medicare beneficiaries represent 70% to 80% of all patients hospitalized with heart failure (HF) each year. The Medicare population has also experienced substantial changes in the epidemiology of HF, with progressively fewer Medicare beneficiaries being diagnosed as having HF each year over the last decade after several decades of increasing incidence. However, the epidemiological mechanisms underlying the observed decline in the incidence of HF are not well understood.
[..] We used a national 5% sample of all fee-for-service Medicare beneficiaries with no prior HF followed up from 2011 to 2016, accessing data on all of the claims submitted to Medicare from inpatient and outpatient encounters, as well as physician or carrier claims.
[..] The primary study outcome was incident HF, which was defined as at least 1 hospitalization with an inpatient HF claim or at least 2 outpatient or carrier HF claims among individuals without prevalent HF. For the latter, we required the outpatient claims to be in 2 separate calendar quarters to limit the selection of individuals who had HF as a potential differential diagnosis rather than a diagnosis of HF that requires longitudinal care. [..] In addition, among those with incident HF on follow-up, mortality within 30 days after the first diagnosis of HF was captured as the secondary study outcome.
[..] there were 1,799,027 unique Medicare beneficiaries at risk of developing incident HF at the beginning of each year during the study period. The median age of this cohort was 73 years (interquartile range, 68-79 years) [..]. A total of 249,832 Medicare beneficiaries in our study cohort had a new diagnosis of HF during the 6-year study period. The prevalence of all 5 risk factors increased over time (0.8% mean increase in hypertension per year, 1.9% increase in diabetes, 2.9% increase in obesity, 0.2% increase in acute MI [myocardial infarction], and 0.4% increase in AF [atrial fibrillation]). The incidence of HF decreased over the study period from 35.7 cases per 1000 beneficiaries (n = 50,946) in 2011 to 26.5 cases per 1000 beneficiaries (n = 37,620) in 2016.
[..] The prevalence of each risk factor (hypertension, diabetes, obesity, acute MI, and AF) increased over time among those with and without incident HF on follow-up. Throughout the study period, the incidence of HF was higher among individuals with vs without each of the risk factors for HF. Of all the risk factors, the incidence of HF was highest among individuals with acute MI and individuals with AF.
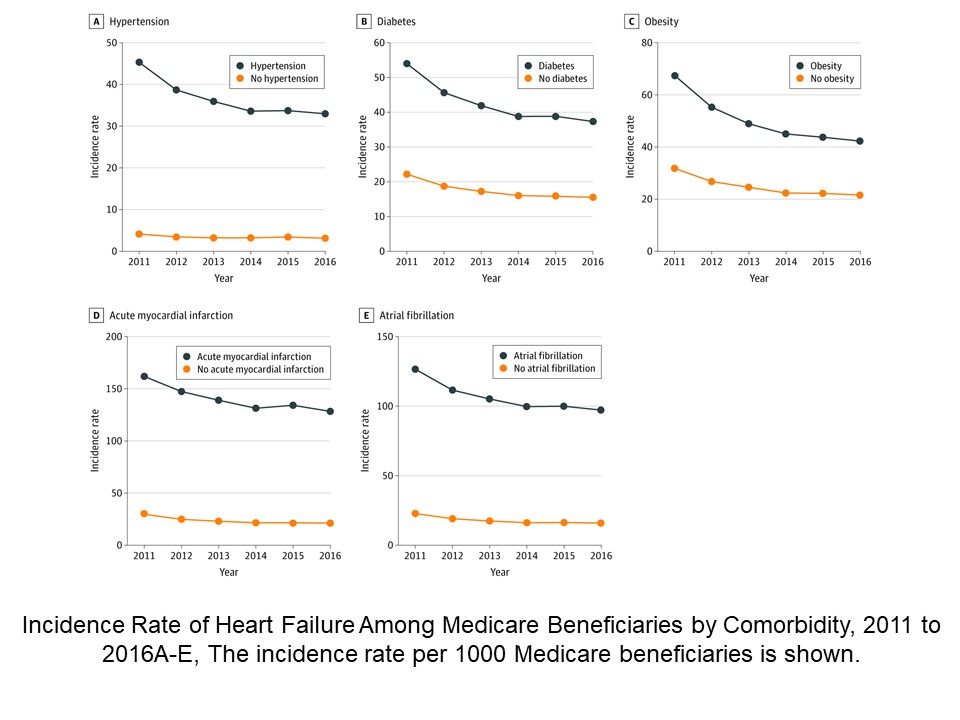
[..] The overall incidence of HF continued to decline between 2011 and 2016, regardless of sex or race/ethnicity. Concomitantly, among individuals with and without HF, rates of key underlying risk factors increased, suggesting that the decline in HF incidence is not because of an overall lower burden of HF risk factors. There was substantial heterogeneity in HF incidence across individual risk factors. Among patients with primary HF risk factors, including hypertension, diabetes, and obesity, the risk of developing new-onset HF compared with individuals without these risk factors decreased over time. In contrast, the risk of developing HF increased in individuals with predisposing CV conditions, such as acute MI and AF, compared with individuals without these conditions.”
Full article, Khera R, Kondamudi N, Zhong L et al. JAMA Network Open 2020.10.23