2020.8.29
“Hearing loss (HL) is an important public health concern, with an estimated 432 million adults worldwide and one-third of people older than 65 years affected by disabling HL. As a noncommunicable disease, HL is far beyond a sensory disorder and can have profound effects on people’s quality of life, which reinforces the importance of early detection and intervention for the maintenance of physical and emotional well-being among older adults, where the burden of disease is the highest.
[..] Eliminating from the categories of self-reported hearing difficulties those that had indicated slight difficulty following a conversation if there is background noise (such as television, radio, or children playing), we had 2249 complete cases with hearing difficulty instead of the initial 3505. This sample size improved the classification accuracy substantially for those with self-reported hearing difficulty, resulting in 9.3% increased sensitivity (79.1%), which refers to the ability of the self-reported measure to correctly identify those with HL (true-positive results). Under that new categorization, 20.9% of those with HL as measured by the handheld audiometric screening device went undetected by the self-reported measure instead of 30.2% (false-negative results: 298 of 1427).
[..] We found that in a population-based sample of 8529 adults 50 to 89 years of age, nearly one-third of those had objectively identified HL that went undetected by the self-report measures.
[..] The existence of objective hearing measures is crucial, particularly for those belonging to high-risk groups that are most likely to remain unrecognized, such as people who face socioeconomic inequalities and adopt an unhealthy lifestyle, because these factors may affect the initiation of help-seeking and consequently the referral to ear specialists.”
Comparison of Self-reported Measures of Hearing With an Objective Audiometric Measure in Adults in the English Longitudinal Study of Ageing, Tsimpida D, Kontopantelis E, Ashcroft D, et al. JAMA Network Open 2020.8.27
“Current clinical trials categorize the severity of heart failure (HF) by the New York Heart Association (NYHA) classification to ensure that enrolled patients have similar disease severity, despite its known limited reproducibility and significant interphysician variability. Alternatively, the severity of symptoms and functional limitations can be directly elicited from patients using the well-validated Kansas City Cardiomyopathy Questionnaire (KCCQ).
For HF with reduced ejection fraction, we used the KCCQ Interpretability study (KCCQINT), an observational registry from February 2001 to January 2002, and the HF-ACTION trial, a trial of exercise training conducted between August 2006 and January 2012. For HF with preserved ejection fraction, we used the TOPCAT trial of spironolactone that enrolled people from August 2006 to January 2012. Because of known concerns about data validity in TOPCAT, patients from the countries of Russia and Georgia were excluded.
[..] Participants with a KCCQ-os score greater than or equal to 80, considered good to excellent self-reported health status, were present in 148 of 546 participants (27.1%) in KCCQINT, of whom 39 (26.4%) were assigned to NYHA class I, 81 (54.7%) to class II, 28 (18.9%) to class III, and none to class IV. Among the 31.8% (677 of 2129) in HF-ACTION with good to excellent self-reported health status, 548 (80.9%) were assigned to NYHA class II, 128 (18.9%) to class III, and 1 (0.1%) to class IV. Among the 23.1% (399 of 1725) with good to excellent self-reported health status in TOPCAT, 340 (85.2%) were coded as NYHA class I-II and 59 (14.8%) were coded as class III-IV.
[..] Given the known interphysician variability in assigning NYHA classes, better categorization of future patients might be achieved with the highly reproducible KCCQ. Some limitations of our study include the age of the studies (although the accuracy of NYHA is unlikely to have changed over time), limited generalizability of examining only 3 studies, and lack of adjustment for other patient factors, although this should not be necessary for 2 assessments of the same underlying construct.
The importance of patient health status has grown, as recently emphasized by the US Food and Drug Administration. Given the marked variability in patient reports of their health status across NYHA classes, future trials should consider patient-reported outcome measures as the basis for defining patient eligibility to enroll a more homogenous cohort of disease severity.”
Comparison of Patient Self-reported Health Status With Clinician-Assigned New York Heart Association Classification, Tran AT, Chan PS, Jones PG et al. JAMA Network Open, 2020.8.28
2020.8.27
“Although aggressive prostate cancer remains the second leading cause of cancer mortality among men in the United States,1 most prostate cancers at diagnosis have relatively low-risk characteristics, with minimal if any probability of distant progression and a natural history measurable often in decades.
[..] surveillance does have its own limitations. Aside from known risks of undersampling higher-risk disease, all established surveillance protocols require repeated prostate-specific antigen (PSA) tests and follow-up biopsies to identify tumor grade or volume progression.5 These biopsies are uncomfortable, expensive, and associated with risks of significant bleeding and infection.
For model validation, we included men undergoing surveillance at the University of California, San Francisco (UCSF) who were not participants in PASS. We again included men diagnosed since 2003 with GG1 tumors on diagnostic biopsy and GG1 or no tumor on confirmatory biopsy.
[..] Final variables independently predictive of reclassification in the multivariable Canary model included maximum percent positive cores (hazard ratio [HR], 1.30 [95% CI, 1.09-1.56]), history of any negative biopsies following diagnosis (1 vs 0: HR, 0.52 [95% CI, 0.38-0.71] and ≥2 vs 0: HR, 0.18 [95% CI, 0.08-0.4]), time since diagnosis (HR, 1.62 [95% CI, 1.28-2.05]), BMI (HR, 1.08 [95% CI, 1.05-1.12]), prostate size (HR, 0.40 [95% CI, 0.25-0.62]), PSA at diagnosis (HR, 1.51 [95% CI, 1.15-1.98]), and PSAk [PSA kinetic measures] (HR, 1.46 [95% CI, 1.23-1.73]).
[..] For prediction of nonreclassification at 4 years after confirmatory biopsy, the AUC was 0.70 (bootstrap-derived 95% CI, 0.63-0.76; P < .001) for the PASS cohort and 0.70 (95% CI, 0.64-0.76; P < .001) for the UCSF cohort.
[..] These results indicate, for example, that men in the lowest decile of risk (risk threshold of 0.08 [10th percentile]) have a negative predictive value of 0.95 (95% CI, 0.89-1.00) for reclassification and that, among men in the lowest quartile of risk (risk threshold of 0.13 [25th percentile]), avoiding all surveillance for 4 years would miss only 29 (95% CI, 16-42) reclassification events per 1000 men. The results were substantially similar for the UCSF validation cohort.
[Click here for the study investigator’s online calculator for risk progression.]
[..] Active surveillance is now endorsed by guidelines on both sides of the Atlantic as the preferred standard of care for most men with low-risk prostate cancer, and data from multicenter registries have confirmed rapid increases in its adoption in US community practice. However, even among the guidelines that now formally endorse active surveillance, only 1 focuses specifically on surveillance and addresses details regarding follow-up protocols. This guideline simply states that serial biopsies should be performed every 2 to 5 years or more often if clinically warranted—a statement based on review of existing protocols rather than on any specific evidence. To our knowledge, no strong evidence or validated clinical tools currently exist to help tailor active surveillance to an individual patient’s reclassification risk.
[..] Our findings suggest that large subpopulations of men eligible for active surveillance could safely adopt a much less intensive regimen after confirmatory biopsy, deferring not only biopsy but also imaging studies and, at least in principle, many interval PSA tests. We stress, however, that the model is not intended to dictate specific care patterns; rather, it is meant to guide discussions between health care professionals and patients regarding how intensively a given tumor needs to be monitored.
[..] under current clinical paradigms, surveillance biopsies cannot be omitted altogether. Many men who are under surveillance in community practice often do not, in fact, undergo confirmatory biopsy or requisite follow-up biopsies, nor even MRI scans intended to serve as surrogates for biopsy (albeit with insufficient data to support such use). A randomized clinical trial of immediate treatment vs monitoring with PSAs alone showed significantly higher rates of disease progression in the monitoring arm. Both the PASS and UCSF protocols specify confirmatory biopsy within 1 year of diagnosis, and our model results may be less applicable for patients with a longer initial interval between biopsies. Hopefully, future subset analyses from this trial and longer follow-up in our cohorts and others will identify some men who need even less frequent or intense surveillance (including eventually monitoring some men with passive watchful waiting). Study results suggest that the Canary model represents a major step toward that goal, providing a tool for dynamic risk prediction and allowing for updating reclassification risks beyond the time of confirmatory biopsy.”
Tailoring Intensity of Active Surveillance for Low-Risk Prostate Cancer Based on Individualized Prediction of Risk Stability, Cooperberg MR, Zheng Y, Faino AV, et al. JAMA Oncology 2020.8.27
2020.8.25
“The proliferation of healthcare apps, potentiated by expanding smartphone ownership and internet connectivity, has been rapid: there are already an estimated 350,000 health apps with 10,000 focused on mental health.
[..] Given the dynamic nature of the digital health app space, it is difficult for service users, peer support specialists, and clinical providers alike to stay updated and ensure that apps are safe, evidence based, usable, and clinically meaningful. As an example of the challenge, a clinically relevant app for depression becomes unavailable and deleted from the app stores every 2.9 days. Providers seeking to utilize apps to support patient management have reservations in recommending apps as a treatment given the limited oversight and accountability that exists with any one app. Complicating matters further, for the general public today, healthcare providers are not the main source of information regarding health apps—individuals are more likely to rely upon app store reviews and rankings to decide on an app for health. However, these app store rankings are marketing metrics not aligned with clinical guidelines or utility. There are mounting concerns about quality and safety even among top-ranked apps in the commercial marketplaces.
[..] The US Food and Drug Administration (FDA) released a set of guidelines for regulating mobile medical apps in 2015. The guidelines impose a thorough set of standards, including those for labeling, medical claims, safety, and effectiveness. Because most apps are categorized as “health and wellness” apps, however, they are not designated as medical devices and thus fall outside the purview of these FDA guidelines. Those which may be medical apps have utilized the regulatory discretion pathway to avoid scrutiny. The app stores, which have emerged as the major sources of information in the absence of FDA assessment, are ill-equipped to provide the thorough expert analysis of accreditation in their current format of user rankings and reviews.
[..] Although there are now upwards of forty-five different frameworks for the evaluation of mobile apps, none of the existing frameworks are suitable for use in health technology assessment (HTA) to inform policymakers, individuals, and providers because they neglect to evaluate both the potential for harm and the effect of software updates. Many of these ranking systems rely upon expert consensus, which can be opaque and difficult to understand for both users and clinicians. Furthermore, there is still significant inconsistency in their outcomes. [..] While the FDA’s Pre-cert initiative holds promise, it is already the topic of political debate and proving its utility, as well as engaging developers may prove to be a slow process. In the meantime, there is a necessity for a framework tailored to clinicians and individuals’ needs today as they determine what apps suit their needs.
We sought to develop a framework for the assessment of health apps that would augment available evaluation models and help individuals harness the potential of digital health by choosing a relevant, safe, and effective app. This model was developed in collaboration with the American Psychiatric Association’s (APA) app evaluation framework and builds off the original model, published in June 2019, and endorsed by the APA in 2017. As the first app evaluation model to be endorsed by a major medical society, the framework reflects consensus from diverse stakeholders including service users, social workers, psychiatrists, psychologists, trainees, and informaticists. However, despite the name there is nothing specific to mental health about the model or its contents; the process of evaluation is suitable for any type of mobile health app. The APA app evaluation model is already well accepted and has been used by the New York Department of Health in the construction of an app library suited to local needs.

[..] While the APA model provides a useful model through which to consider health apps and make informed decisions, it may be overwhelming for a single clinician during a short clinical visit to attempt to rigorously analyze the many apps that may be relevant to an individual with a particular condition and preferences. To make this framework functional and actionable for the public use, we adapted the questions for inclusion in a database. Each question was operationalized so that answers are binary or numeric, permitting objectivity. This resulted in 105 questions. In contrast to many existing frameworks and rating systems, many of which rely upon subjective quality and perceived impact, the assessment of an app is intended to be data-driven rather than derived from ratings of expert consensus.
An additional benefit of the 105 objective questions is the opportunity for crowdsourcing. Since there is no qualitative assessment involved, there is great potential to involve many people in the evaluation process and offer clear quality controls. This crowdsourcing is an integral component of maintaining an up-to-date and thorough database that reflects the wide-reaching, fast-moving nature of the mental health app space. In order for rapid knowledge synthesis to be obtained from crowdsourcing, the information needs to be accessible, cost-effective, and scalable. Creating such a crowdsourced model offers the advantage of involving all stakeholders, encouraging diversity, and quickly identifying unsafe apps as outlined in our group’s recent proposed around regulating digital health technologies with transparency.
[..] Although there are questions pertaining to each level of the pyramid (access/functionality, privacy, evidence, usability, interoperability), additional questions were added by a team of researchers to highlight further data that can be objectively coded about apps including data input methods, app outputs, and engagement styles offered. These questions were derived from prior research examining how attributes of top-rated apps relate to quality and refined through consensus in rating over 100 apps with them. Further feedback was sought from end users and clinicians to refine the clarify and focus of these questions. Consensus was obtained from twenty individuals who rated at least two apps and participated in focus groups to offer feedback on the process. While answering 105 questions about an app is of course not a rapid process, the end product of an easily searchable and updatable database enabling users to immediately sort apps according to the presence or absence of different features relevant to each unique clinical case is appealing. As with the APA model, there is no single score assigned to an app; rather, the database enables customization in consideration of various app aspects.”
Actionable health app evaluation: translating expert frameworks into objective metrics, Lagan S, Aquino P, Emerson MR. npj Digital Medicine 2020.7.30
“There is an opportunity for connected diabetes care—virtual diabetes management programs rooted in smartphone technology, connected devices for blood glucose monitoring, and remote coaching or support—to fill gaps in care access and quality. [..] To date, connected care programs have more commonly reported group differences in HbA1c in pre-post analyses in the absence of comparator groups. One reason for this observation may be the extended timeline of prospective, randomized outcomes trials, which does not align well with the iterative digital health development cycle. Pragmatic, observational, and registry studies with real-world data will be key to fully assessing the benefits of specific connected care offerings. Still, as these programs evolve, they have the potential to drive better population diabetes outcomes by: (1) filling temporal and comorbid gaps in care; (2) decentralizing and scaling expert care; (3) providing self-management support to reinforce healthy behaviors; and (4) using a data-driven approach to recommend therapies (i.e., medications, technologies, and programs) to the right person at the right time.
Classification of connected diabetes care programs
| Care team composition | Estimated relative cost | Likely target user | Examples | |
| Virtual diabetes clinic | All clinicians, including physicians, nurse practitioners, and physician assistants | Highest | Highest-risk, highest-cost patients who are furthest from target and need frequent therapeutic adjustments | Virta, Onduo |
| Non-physician clinician-driven | All clinicians, excluding physicians, nurse practitioners, and physician assistants | High | High-risk patients who (a) have access to high-quality, frequent in-person care and/or (b) are on a fairly stable and successful therapeutic regimen | Livongo Health, mySugr, Omada Health, One Drop, Cecelia Health (soon aims to be Virtual Diabetes Clinic), Vida Health, Noom, Dariohealth, Canary Health |
| Artificial intelligence coach | Automated coaching | Low | Members of large employer/health plans who prefer daily engagement/coaching and do not need frequent therapeutic adjustments | Welldoc, Lark Health |
| Software tools | Brick-and-mortar clinicians | Low | Everyone with a diabetes or prediabetes diagnosis and a brick-and-mortar clinician | Glooko, Tidepool, Fitbit (Twine Health), device manufacturer software, specific EHR modules |
| Quantified self solution | None | Middle | Motivated people who may be at risk of developing disease | UHC Motion Program, Devoted Health Medicare Advantage, Aetna Attain |
[..] Some NPCD [non-physician clinician-driven] connected diabetes care organizations have opted to partner with established, large-scale telemedicine providers such as Teladoc, Doctor on Demand, and MDLive. This arrangement may offer the possibility of non-physician clinicians quarterbacking the bulk of care and referring out for a telemedicine consult when necessary, allowing for medication optimization and medical device prescription similar to that seen in a vertically integrated virtual diabetes clinic. This presumably decreases cost of operations for the connected care organization but may reduce the level of care coordination, quality, and continuity as the consulting physician is not fully ingrained in the patient’s care team. It is unclear if there will be a difference in the quality of care provided or patient outcomes between these two strategies, though we look forward to future analyses comparing relevant quality metrics between the two approaches for similar populations.
[..] Software tools can help brick-and-mortar clinicians more effectively manage populations of people with diabetes. They also provide a secure, low-hassle means of monitoring and communicating with patients between clinic visits. Software tools can also potentially help HCPs to expand their patient panel, though probably not to a significant enough extent that dedicated remote care teams are no longer needed. There are, however, three notable challenges with these software tools: (1) Health systems need to develop efficient workflows that ensure all clinicians practice at the top of their licenses and that physician and NP time is optimally leveraged to serve a large panel size; (2) Not all are currently embedded in the electronic health record (EHR), forcing clinicians to navigate multiple interfaces; and (3) Time spent using these tools is not currently reimbursed but can generate additional work for the provider team (in their current form). Payment reform toward a more capitated or outcomes-based system could allow health systems to reorganize staff, care delivery, and compensation to incentivize optimal utilization of these software tools.”
A care team-based classification and population management schema for connected diabetes care, Levine BJ, Close KL and Gabbay RA. npj Digital Medicine 2020.8.7
“In 2008, the Centers for Disease Control and Prevention Select Panel of Preconception Care identified more than 100 risks that, if identified and interventions are initiated before pregnancy, could improve maternal and infant birth outcomes.
[..] Health information technology offers a promising way to engage women in preconception care. Embodied conversational agents (computer-generated characters that simulate face-to-face conversation and communicate key health messages) are a new technology with the potential to overcome barriers to providing health education and counselling.
[..] We designed and tested an embodied conversational agent, called Gabby, to deliver simulated preconception care to women. Gabby delivers a preconception care risk assessment that screens for 102 health risks, and provides tailored advice. Gabby then asks women to select the risks they want to discuss, describes why the risk is important and offers suggestions about how to take action on it. During up to 12 months of subsequent interactions, Gabby identifies the degree of progress, provides feedback on actions taken, reassesses readiness, and recommends next steps. The system assesses a woman’s understanding and recall, repeating information as necessary, and using non-verbal conversational behaviours, such as hand gestures and facial expressions. The woman engages by selecting a response from a multiple-choice menu updated at each turn of dialogue. Gabby creates a customisable list of identified preconception care risks, called the my health to-do list, to assist in tracking progress.

[..] We assessed progress using the transtheoretical model of health behaviour change, which describes health behaviour change as a process, rather than a single event with stages of change, that are precontemplation, contemplation, planning, action, and maintenance. Research has shown dramatic improvements in health behaviours using stage-matched interventions. For women in precontemplation, Gabby uses motivational interviewing to assist the woman to recognise her ambivalence and take the first steps to address a particular risk or behaviour. Other behaviour change techniques are used for individuals in later stages of change, for example, a woman in contemplation is provided shared decision making to help decide which alternative method is best for her. Goal setting and positive reinforcement are used for behaviours requiring incremental, longitudinal change, such as exercise and diet.
[..] We report the results of a randomised controlled trial with 1-year follow-up to examine the effect of Gabby on preconception care risks in a sample of 528 African American and Black women recruited from 35 states and 242 cities in the USA.
[..] All research participants were emailed an internet link and secure login to the Gabby system, which provided access to the baseline risk assessment. Participants were presented with a personalised list of risks identified on the risk assessment and asked to assign each risk with one of the five stages of change corresponding to the transtheoretical model.
The 102 risks assessed within the study were grouped under 13 domains: emotional and mental health, environmental issues, genetic health history, health care and programmes, health conditions and medicines, immunisations and vaccines, infectious diseases, men and health care, nutrition and activity, relationships, reproductive health, substance use, and family planning. For 76 of 102 risks, the behaviour associated with forward (or backward) progress on the transtheoretical model was the discussion of that risk with a clinical provider (eg, talking with a clinician about the risks of sickle cell disease to a future pregnancy or about receiving the human papillomavirus immunisation to prevent cervical cancer). For 26 of 102 risks, the behaviour associated with that risk required working with Gabby on longitudinal behaviour change activities, such as motivational interviewing that do not necessarily require a clinical visit (eg, eating a healthier diet, exercising more, or smoking cessation).
At months 6 and 12, all participants were contacted by email, presented with a survey including a personalised list of risks that were identified on the baseline risk assessment, and again asked to label each risk with one of the five stages of change. A telephone call was then scheduled with all participants to collect any remaining outcome data. During this data collection, participants were asked about their health-care use. Intervention participants were asked to rate their satisfaction with Gabby using six questions asking about ease of use on a 1 (easy) to 7 (difficult) scale, trust in Gabby on a 1 (very much) to 7 (not at all) scale, and then four (yes or no) questions asking: Did Gabby answer your questions? Were there issues about your health that you were not comfortable telling Gabby? Have you already made health changes based on recommendations provided by Gabby? and Based on your conversations with Gabby, will you make changes to your health in the future?
[..] From March 11, 2014, through July 8, 2017, 938 women contacted research staff, 410 were excluded and 528 were recruited and consented from 35 states and 242 cities across the USA. 262 participants were allocated to the intervention group (Gabby) and 266 to the control group. 6-month data were obtained for 223 Gabby and 227 control participants, and 12-month data for 232 Gabby and 232 control participants. 6-month data for at least one identified risk behaviour was obtained for 131 Gabby and 156 control participants, and 12-month data, concluding on April 30, 2018, was obtained for 116 Gabby and 116 control participants.
[..] The participants were a mean age of 27 years (Gabby 27·5 years, control 27·3 years), 407 (77%) of 528 were a student or worked full time or part time, 465 (88%) of 528 attended some post-secondary school, 141 (42%) of 333 reported having been pregnant at least once, 503 (95%) of 527 used the internet to learn about health, and most had high health literacy, social support, and self-efficacy.
[..] A mean of 21 risks (SD 9·7) were identified in the Gabby group and 22 (10·1) in the control group.
[..] On average, women interacting with Gabby for 12 months reported reaching the action or maintenance stage of change for 56·0% (SD 27·5) of risks identified compared with 50·9% (29·4) in the control group (IRR 1·17, 95% CI 1·08–1·27).
[..] Among women using Gabby, the risks most often progressing to action or maintenance were having a discussion with their clinicians about sexually transmitted infections, ethnicity-based reproductive risks, and working to improve their diet.
[..] When analysing only the intervention group, each additional login was associated with an average increase of 0·9% in the reported rate of achieving action or maintenance at 12 months compared with baseline (p<0·0001). This result remained significant when controlling for education, income, REALM score, experience with computers, attitude towards computers, access to computers, and intention to become pregnant.
[..] After 12 months, 199 (76%) of 262 women in the intervention group interacted with Gabby at least once, and the median number of logins was six (IQR 8). A session lasted a mean of 14·5 min (SD 6·3). The total average interaction time (not including the risk assessment) per woman using Gabby was 123·5 min (155·0).
[..] Participants in the intervention group reported fewer total clinical visits at 12 months than participants in the control group (587 vs 812, respectively; p=0·02). In the Gabby group, compared with the control group, there were fewer visits to the emergency room (27 vs 51, respectively; p=0·02), specialty visits (91 vs 165, respectively; p=0·001), and mental health visits (182 vs 235, respectively; p=0·27).
[..] While most women and physicians understand that preconception care is important, it remains challenging to engage women in this care, and difficult for health professionals to deliver the broad array of these services. Alternatives are needed. Embodied conversational agents like Gabby have been shown to be acceptable to patients, easy to use, and effective, particularly among those with inadequate health literacy. Scalable health information technology like Gabby could be impactful as a population health tool to assist health systems to deliver preconception care to eligible women. Gabby could also be used to assist busy clinicians, as an adjunct to office-based encounters, by informing women about their preconception care risks before a visit, and allowing the woman to bring her list of risks (the “my health to-do list”) to her provider, resulting in a more patient-centred discussion.
Systems like Gabby can directly address clinician time restraints. Among women using Gabby, there was an average of six interactions over 2 h provided at times chosen by, and convenient for, the woman over 12 months. This far exceeds the typical 15 min clinical encounter that is provided during an annual visit.
[..] the risks identified are not of equal importance, and achieving action and maintenance is not equally meaningful. To date, studies have not shown the relative risk of birth outcomes for all preconception care risks. However, our results show that the intervention has a consistent impact across clinical content areas, and is not predominated by those risks that are easily changed or have less clinical impact than others. However, the intervention showed notable, although not statistically significantly, impacts in several domains that might be due to lack of statistical power and small within-domain sample sizes.
[..] the absolute difference in achieving the action and maintenance stage of change is statistically significant, but it is unclear if an absolute difference of 7·3% is clinically significant. While similar magnitudes of reaching action or maintenance for behavioural variables have been reported, there have not been studies reporting such a large number of heterogeneous risks. It is an assumption that reducing these risks will improve clinical outcomes, such as the rates of preterm delivery or low birthweight; however, having such a significant portion of the study population achieve action or maintenance on important health risks independently endorsed by expert groups has implications for improving the health of mothers and infants.”
Improving the health of young African American women in the preconception period using health information technology: a randomised controlled trial, Jack BW, Bickmore T, Yinusa-Nyahkoon L et al. The Lancet Digital Health, 2020.9.1
2020.8.24
Excerpt – “legal determinants of health,” namely how law can address underlying causes of premature mortality, merit examination and consideration. Cost-effective evidence-based laws can safeguard the public’s health, reduce disparities, and extend life expectancy across socioeconomic groups, especially in disproportionately affected regions of the US. Despite their promise, public health laws are underutilized.
[..] Life expectancy gaps among the richest and poorest 1% of the population are estimated to exceed 10 years for women and 14 years for men. Stated simply, poorer, less-educated individuals in the US live considerably shorter lives. This pattern of inequality has been highlighted further during the COVID-19 pandemic.
[..] Greater uptake and uniformity of effective legal measures across the US could likely reduce morbidity, promote health equity, and increase life expectancy. These benefits, moreover, are often achievable without substantial increases in public sector funding. Given the effectiveness and potential cost savings of these legal measures, legislators and policy makers should consider evidence-based laws to ameliorate population health and social justice, especially in regions where life expectancies have declined significantly. Yet, substantial challenges remain.
In a federalist society, states and localities can be incubators for progressive laws with corresponding benefits. Yet, variations in legal innovations lead to uneven applications of evidence-based laws and geographic disparities in key health indicators, as seen in varying state and local responses to COVID-19. Federal inaction can perpetuate legal inconsistencies in socially controversial spheres, including firearms, reproductive health, and commercial taxation and regulation (eg, alcohol, tobacco, vapes, opioids).
Worse still, federal and state authorities increasingly preempt lower-level public health laws, sometimes penalizing noncompliant officials. Such measures impede grassroots initiatives in food and nutrition, environment, or consumer litigation, essentially cutting off legal options in states most adversely affected by diseases of despair. Corresponding legal voids may go unfilled (eg, national firearm background checks). Core public health funding is also incommensurate with population health needs. Even as life expectancy decreases, support for public health systems and the role of law are undervalued by some policy makers and citizens.
Previous findings on declining life expectancy in the US should reset national health priorities warranting concerted responses. This requires private sector responsibility (concerning food, alcohol, tobacco, pharmaceuticals, and health care), social mobilization for a healthy life span, and public health legal interventions. Evidence-based cost-effective laws can improve social determinants and help reverse ongoing declines in health and longevity.
[From the editorial’s supplement]
| Issue | Citation | Potential mechanism for reducing morbidity or mortality | Assessments or findings |
|---|---|---|---|
| Opioids | |||
| Increase access to naloxone | Utah Code Annot § 2655-105 (2016) | Reversing effects of opioid overdoses via (1) standing orders for pharmacist dispensing of naloxone; and (2) Good Samaritan protections for prescribing, dispensing, and administering | Assessment of population in 50 states and DC from 2000-2014 found that a combination of naloxone access and Good Samaritan laws was associated with decreases in OUDs compared to states lacking similar laws. OUDs increased from 2.71/100 000 persons in 2000 to 8.43/100 000 persons in 2014. Among states with naloxone access laws, however, OUDs decreased by approximately 14% (P = .033), or 1.18/100 000 persons, over this same period. Among states with Good Samaritan laws, OUDs decreased by approximately 15% (P = .050), or 1.26/100 000 persons, over this same period. Among African Americans, OUDs decreased by 23% (P = .001), or 1.94/100 000 persons, and 26% (P < .001), or 2.19/100 000 persons, respectively |
| Authorize OAT | 12 Virginia Admin Code § 30-130-5000 et seq (2017) | Reducing mortality risks for persons with opioid use disorder by removing barriers or increasing access to OAT involving methadone and buprenorphine | Comparison of 17,568 Massachusetts adult overdose survivors from 2012-2014 found OUD decreases over a year-long assessment compared to those not receiving medication assisted treatment. All-cause mortality among the study group was 4.7 deaths (95% CI, 4.4-5.0 deaths) and opioid-related mortality was 2.1 deaths (95% CI, 1.9-2.4 deaths) per 100 person-years. Among persons enrolled in methadone maintenance treatment (11.6% of cohort, or 2040 persons), decreases were measured in all-cause mortality (AHR, 0.47; 95% CI, 0.32-0.71) and opioid-related mortality (AHR, 0.41; 95% CI, 0.24-0.70). Among persons receiving buprenorphine (17.2% of cohort, or 3022 persons) decreases were measured in all-cause mortality (AHR, 0.63; 95% CI, 0.46-0.87) and opioid-related mortality (AHR, 0.62; 95% CI, 0.41-0.92) |
| Alcohol | |||
| Increase state alcohol sales tax | Maryland Code Ann, Tax General § 11104(g) (2011) | Lowering excessive alcohol consumption and related harms via increase of state tax on sales of alcoholic beverages | Over a 29 mo period a 50% increase in alcohol sales tax (from 6% to 9%) led to a gradual annual reduction of 6% (P < .03) in monthly rates of alcohol-positive drivers (n = 34 098) involved in injury collisions from 227.661 drivers per month from January 2001-July 2011 (n = 28,906) to 179.03 drivers per month from August 2011-December 2013 (n = 5192) |
| Reduce density of alcohol outlets | San Francisco Planning Code Art 7 § 781.9 (2019) | Diminishing density of alcohol outlets and consequent reduction in excessive alcohol consumption and related harms | A 2009 meta-analysis of several time-series studies of alcohol outlet density changes concluded density limits may be associated with reducing alcohol consumption and medical and other harms (eg, domestic violence, public nuisances, loitering, vandalism, and other crimes) |
| Tobacco | |||
| Smoke free | Wisconsin Stat § 101.123(2)(a) (9) (2010) | Cutting tobacco use among persons in employment or other public places where primary and second-hand smoke impacts persons’ respiratory health | A study of 531 bartenders within 3-6 mos after 2010 implementation of legal antismoking intervention observed a significant decrease in 8 upper respiratory symptoms among non-smoking bartenders (eg, reported 9% decrease, from 37% to 28% (P = .003), in “‘wheezing or whistling in the chest’” and a 16%, decrease, from 54% to 38% (P = .000), in morning coughing) |
| Tobacco tax | CHIP Reauthorization Act of 2009, 26 USCA § 5701 (2009) | Decreasing smoking initiation among youth users as well as past-month smoking | Examination of smoking behaviors of youth/young adults from 2002-2011 showed a 2009 federal tax of .62 cents per cigarette pack was associated with reducing average rates of smoking initiation from 6.7% before the tax increase to 5.1% afterwards. The average rates of youth (aged 12-17) past-month smoking at 10.9% decreased to 8.3% after the tax increase. Odds for both decreased (OR = 0.83, P < .0001) |
| Firearm violence | |||
| Universal background checks | California Penal Code § 28050 (2012) | Reducing homicide rates through firearm background checks at point of purchase or via license/permit application | After simultaneously controlling for 10 state firearm laws in 50 states from 1991-2016, universal background checks were associated with a 14.9% (95% CI, 5.2%-23.6%) reduction in homicide rates |
| Violent misdemeanor laws | Hawaii Rev Stat Annot § 134-7 (2013) | Lessening homicide rates through prohibitions of firearm possession among those committing violent misdemeanors | After simultaneously controlling for 10 state firearm laws in 50 states from 1991-2016, violent misdemeanor laws were associated with a 18.1% (95% CI, 8.1%-27.1%) reduction in homicide rates |
| Suicide | |||
| Extreme risk protection orders | Indiana Code § 35-47-14 (2016) | Lowering suicide rates through the seizure of firearms from individuals deemed a threat to themselves or others | Examination of 14 suicide outcomes from 2006-2017 for 395 gun-removal actions showed the proportion of suicides by men involving guns (7 out of 14) decreased compared with the portion of suicides by men involving guns in Indiana’s general population (50% vs 58%, respectively) and was lower than expected among firearm owners (65% or higher). Based on comparable case fatality rates, 1 firearm-related fatality was prevented for every 10.1 firearm removal actions |
| Suicide prevention training | Garett Lee Smith Memorial Act, 42 USCA § 290bb-36 (2016) | Reducing suicides and attempts via funds and technical assistance for states to train those in contact with adolescents to identify high risk youth and offer treatment or service referrals | Assessment of 466 counties implementing program activities from 2006-2009 found significantly lower suicide attempt rates (4.9 fewer attempts per 1000 youths) among 16-23 y olds in the following year compared to 1161 similar counties not implementing such activities. Between 2008-2011 more than 79,000 suicide attempts may have been averted |
| Obesity/hypertension | |||
| Taxing sugar-sweetened beverages | Berkeley City Ordinance # 7388-N.S. (2015) | Diminishing obesity and related diseases by decreasing consumption of SSBs | Assessment of SSB tax between 2014-2017 concluded that consumption decreased in demographically-diverse Berkeley neighborhoods by 0.55 times per day with residents reporting drinking 52% fewer servings (from 1.25 to .70 servings per day) after passage compared to pre-tax consumption in 2014 |
| Food nutrition in schools | Child Nutrition & WIC Reauth Act of 2004, 42 USCA § 1751-1769j (2004); Healthy, Hunger-Free Kids Act of 2010, PL # 111-296, 124 Stat 3138 (2010) | Reducing obesity and hypertension risk through school food nutrition policies to lower increases in BMI | An evaluation of 211 5-8th grade students in 12 school districts from 2011-2015 attending schools receiving federal technical support for nutrition programs found (1) less frequent consumption of SSBs (37.95% vs 27.18% of students drank SSBs on 2 or fewer days in the past 7 d; OR = 1.36, P = .025) by the end of the study. Students were also less likely to have an increase in BMI (of less than 1% vs 2%-3%) compared to 193 students at schools not receiving technical support |
| Posting calorie information | NY City Health Code § 81.50 (2016) | Requiring chain restaurants to post calories for standard menu items | Assessment of health data from 61 New York counties from 2004-2012 showed that calorie labeling requirements were associated with a 3.0% decrease (or .818 actual difference) in average BMI among adult populations in 11 counties (BMI mean of 26.790) compared to adult populations in 50 counties (BMI mean of 27.608) that had not required calorie labeling |
| Social determinants | |||
| Expanding health care access | Affordable Care Act, 42 USCA § 1396a(a) (10)(A)(i) (VIII) (2010) | Addressing racial disparities via enhanced health care coverage provisions that increase access to care | Examination of ACA’s major coverage provisions found a reduction between 2013-2015 in average national racial disparities between Whites and Hispanics and Whites and African-Americans regarding: (1) percentages of uninsured working adults, (2) persons skipping needed care due to costs, and (3) persons lacking a usual provider. Even greater decreases were measured in Medicaid expansion states. Compared to 2013, the overall decline in the uninsured rate amounted to an estimated 2 million more African American adults and an estimated 3 million more Hispanics obtaining health insurance |
| Minimum wage laws | New York Laboratory Law § 652 (2016) | Decreasing STI rates through minimum wage increases | A nominal $1.00 increase in the adjusted minimum wage between 2003-2015 was associated with a decrease in some STI rates among women living in 66 large metropolitan areas (19.7% decrease in syphilis from .30 cases per 100 000 to .27 cases per 100 000 cases; 8.5% decrease in gonorrhea infections resulting in 11 fewer cases per 100 000 from 2003 to 2015) |
Abbreviations: AHR, adjusted hazard ratio; BMI, body mass index; OAT, opioid agonist therapy; OR, odds ratio; OUD, opioid overdose deaths; SSB, sugarsweetened beverage; STI, sexually-transmitted infection.
Legal Interventions to Address US Reductions in Life Expectancy, Gostin LO, Hodge JG and Levin DE. JAMA 2020.8.24
“Chow and colleagues confirm that cardiovascular events are an important contributor to the morbidity and mortality associated with influenza. They studied 80,261 adults with confirmed influenza and determined that almost 12% had an acute cardiovascular event, most commonly acute heart failure (6.2%) or acute ischemic heart disease (5.7%). This study also showed that patients with the combination of influenza and acute cardiovascular events have high care needs: Median length of stay was 5 days, 31.2% of patients required intensive care, and 7.3% died in the hospital. Of fatal cases, 1 in 4 had an associated acute cardiovascular event, reflecting potentially preventable influenza-related cardiovascular mortality.
[..] Unlike children, in whom fever is common with influenza, only 30% of adults with influenza have fever. Thus, influenza may go undiagnosed unless tested for regardless of fever. Diagnosis allows early commencement of antiviral therapy, which may mitigate potential complications. In 1 study, oseltamivir reduced the rate of cardiovascular events from more than 20% to 8.5%.
[..] Chow and colleagues showed that vaccination was beneficial even when it did not prevent influenza. Among study patients hospitalized with influenza, those who were vaccinated were significantly less likely to develop acute heart failure and acute ischemic heart disease than those who were unvaccinated. This finding shows that the benefit of influenza vaccination extends beyond simply preventing infection—influenza vaccination prevents severe complications of infection when infection occurs despite vaccination. Cardiovascular disease is the leading cause of morbidity and mortality globally, so by preventing a proportion of acute cardiovascular events, influenza vaccination will have a substantial public health benefit and will likely be cost-beneficial.
[..] The estimated efficacy of influenza vaccines for secondary prevention of cardiovascular events is 15% to 45%, similar to that of statins, antihypertensive agents, and smoking cessation.”
Influenza Vaccine: Routine Secondary Prevention for Patients With Cardiovascular Disease?, MacIntyre CR. Annals of Internal Medicine, 2020.8.25
“The article by Bruch and colleagues adds another specialty to the list of physician specialty areas—notably dermatology and ophthalmology—for which recent articles have described private equity activity. We can anticipate that additional reports of growing private equity acquisitions in other specialties (eg, gastroenterology) will soon follow. Articles to date are similar in 3 ways. First, they report rapidly increasing private equity acquisitions in a given specialty. Second, they report a similar private equity modus operandi across specialties: acquire a relatively large platform practice [..] in a given geographic area, then acquire smaller practices in that area and group them into the same organization as the platform practice; use debt to finance the acquisitions and assign that debt to the acquired practices; find ways to increase net revenue from the agglomerated practices; and sell the agglomerated practices within 3 to 5 years for considerably more than the price paid by the private equity company. Third, the articles [..] lack data on the performance—in quality and cost of care, or in physician or patient satisfaction, of private equity-owned practices.
[..] Opponents of private equity argue that the intense pressure on firms to generate returns for their investors (private equity firms generally project a return of 20% annually averaged across the 3 to 5 years before a practice is sold) is not compatible with putting patients’ interests first and not compatible with physician professionalism and its commitment to put patients’ interests first.
[..] it is likely that in private equity acquisition of physician practices, as in other areas of life, there are good actors and bad actors, and competent and not-so-competent firms. It remains to be seen whether physicians, patients, or health insurers will be able to discriminate among them. But that has always been true as well for practices owned by physicians or hospitals.
[..] For better or for worse, the United States is moving from a system based on small, independent physician practices to physicians being employed by large corporations (including hospital systems, health insurers, and private equity firms), from small, independent community hospitals to multihospital systems (including hospitals owned by private equity firms), and from small, not-for-profit health insurers to a small number of very large national and regional insurers.
[..] Neither patients nor anyone else are likely to realize if a small practice is delivering inferior care (the practice’s physicians may not realize it either), and/or that the practice’s physicians place profit over patients. The large number of physicians and staff involved in corporations that employ physicians are likely better equipped to identify and do something about physicians who consistently deliver poor care. Corporations also have the capital to invest in executives whose job is to improve the care the corporate practices provide and in systematic processes to improve quality. Corporate medical practices are more likely to score well on the limited measures of quality of care that are currently in use; it is not known whether they provide better quality than independent practices in the numerous important areas of quality, such as accurate diagnosis, that are difficult or impossible to measure. Finally, the economic power of large corporate organizations in medical care can translate into political power, which can help preserve or enhance their economic power. This was recently evident when national physician staffing companies that employ physicians in anesthesia, emergency medicine, neonatology, radiology, and other hospital-based specialties used their financial might to block surprise billing legislation in Congress.”
Private Equity, Women’s Health, and the Corporate Transformation of American Medicine, Casalino LP. JAMA Internal Medicine, 2020.8.24
2020.8.22
“Medicaid expansion is associated with earlier presentation for surgical conditions, access to rehabilitation services after trauma surgery, and increased use of joint replacement surgery. Most of the literature regarding Medicaid expansion has focused on the inpatient setting; yet, understanding the association of Medicaid expansion with outpatient surgery is important because ambulatory surgical procedures are often more cost-effective compared with procedures performed in the hospital setting, and low-income populations have historically had limited access to ambulatory surgery.
The Lin et al study used a robust quasi-experimental design to report that more low-income Americans had access to ambulatory surgery [specifically, laparoscopic cholecystectomy, breast lumpectomy, laparoscopic hernia repair and open hernia repair] in states that expanded Medicaid coverage. Notably, in the case of breast lumpectomy, there was also data to indicate a spillover effect. The receipt of breast lumpectomy increased among both uninsured and privately insured patients in expansion states compared with nonexpansion states.
[..] the most important unanswered question is whether this increase in ambulatory surgery use represents meaningful improvements in access to care and health outcomes. The most powerful evidence of improvement would be reductions in morbidity, and even mortality, among patients who received outpatient surgical care in expansion states. Because the study was based on data from outpatient surgical care use alone, it is not possible to assess subsequent consequences. We also cannot discern whether the increase in ambulatory procedures was associated with medical necessity or whether other forces were at work, such as moral hazard on the part of patients or health care professionals. To answer these questions, future investigations can combine ambulatory data with data on inpatient surgical care, self-reported access to surgical care and quality of life, and long-term outcomes, such as cancer mortality and all-cause mortality.”
Affordable Care Act Medicaid Expansion and Access to Outpatient Surgical Care, Goldman AL, Paasche-Orlow MK and Drake FT. JAMA Surgery 2020.8.19
2020.8.21
“The Choosing Wisely movement is an attempt by numerous medical societies—led by the American Board of Internal Medicine Foundation—to curtail medical services that provide limited benefits relative to their costs. However, Choosing Wisely demonstrates the drawbacks of such a movement that does not account for liability considerations, which may help to explain why the uptake of Choosing Wisely recommendations has not been more robust.
[..] One study found that when providers faced no threat of liability, inpatient spending was 5% lower while patient outcomes remained the same, suggesting the potential for substantial savings.
First, clinical uncertainty calls into question what constitutes sound medical practice and challenges the very idea of a consensus-driven standard of care. While the standard of care may be clear in some instances, the appropriate course of action in each situation is often unclear, as evidenced by wide variations in treatment patterns across the country.
[..] Customary practice is determined by a jury’s interpretation of often-conflicting expert opinion on how providers in a given area deliver care. It offers uncertain guidance to providers in specific circumstances and undermines a fundamental principle of medical malpractice law—that the standard of care should be scientifically determined by medical experts. Given clinical uncertainty, providers are incentivized to practice defensively, potentially ordering unnecessary tests or procedures.
Second, the post hoc evaluation of providers’ actions creates structural uncertainty. The standard of care is not determined until well after the actions giving rise to a malpractice claim have occurred. Providers often do not know what standard their actions must satisfy at the time of the clinical encounter. Clinical and structural uncertainty may leave providers unsure of what to do when delivering care.
Malpractice reform has generally taken a remedy-centric approach, focusing on the amount of damages awarded. Such reforms do little to provide clinicians with better information about the proper course of action in any given case. Recent research demonstrates that changes to the standard of care can induce clear changes in clinical practice. Focusing on the determination of liability, instead of remedies, may be better at reducing defensive medicine and its associated costs.
As a policy alternative, we advance the concept of Safe Harbors, which offer providers guidelines for delivering care in specific targeted situations and, if followed non-negligently, can immunize providers from liability.
[..] Effective Safe Harbors require 3 critical characteristics. First, Safe Harbors must be announced in advance so providers can deliver care with the relevant standard in mind. Second, each Safe Harbor must provide clear, narrow, and targeted guidelines. Though not yet operationalized, such guidelines would reduce the use of discretion and thereby prevent courts and juries from second-guessing the appropriateness of a provider’s actions. Special guidelines of this type also return standard-setting to medical experts, diminishing the role of courts and lay juries.
Third, the guidelines must carry the force of law and constitute the standard of care, not merely provide evidence of the standard. If a guideline is not the standard, then providers will face uncertainty over how a court or a jury will apply a standard. Choosing Wisely has offered numerous recommendations, but those recommendations do not carry the force of law.
[..] Safe Harbors could be implemented by Quality Improvement Organizations (QIOs), which operate under federal law as self-regulatory organizations designed to monitor quality and cost in federal health care programs. The QIO legislation includes a provision that immunizes providers from malpractice liability when they practice nonnegligently in conformity with a standard approved by a QIO. Quality Improvement Organizations are authorized to engage in general quality-of-care review in which they can endorse Safe Harbors for narrowly defined areas of care.
Constraints on Medical Liability Through Malpractice Safe Harbors, Blumstein JF, Michael BJ and Storrow AB. JAMA Health Forum 2020.8.14
2020.8.20
“In most states, private for-profit plans are the dominant option and sometimes the only choice. When there is an alternative to a for-profit plan within a state, the option is almost always a nonprofit plan rather than a public plan. California is unique in that in 13 counties, accounting for nearly 8 million Medicaid beneficiaries, for-profit plans compete directly with county government–operated public plans. This provides a natural experiment to evaluate the performance of public vs for-profit plans in the care they provide to Medicaid beneficiaries.
[..] In every California county in which there is a choice, enrollment in the public plan is higher than in the for-profit plan. [..] As of July 2020, there were 5.1 million beneficiaries enrolled in the public plans and 1.6 million enrolled in the for-profit plans in the 13 counties with a choice of both. In fact, the only way that for-profit plans have increased market share in California over the past decade is by expanding into counties where there is no public option. Incidentally, in counties lacking a public health plan option, the quality of care for Medi-Cal beneficiaries as measured by HEDIS and CAHPS is significantly worse than in counties that offer public health plan options.”
Medicaid’s Public Health Plan Options, Bindman A. JAMA Health Forum 2020.8.20
“Even with external incentives, social needs screening has not exactly been embraced by providers: only 16% of physician practices and 24% of hospitals currently screen for key social risk domains. Perhaps more importantly, “screen and refer” programs have had low uptake by patients and minimal effect on outcomes.
[..] Social needs screening probes the most private and potentially stigmatized areas of patients’ lives, including poverty, racism, and intimate-partner violence. Screening without careful deliberation can harm patients through trauma, discrimination, or legal consequences such as loss of child custody or deportation. [..] when clinicians are not able to offer effective solutions to patients who disclose dire needs, they may set unrealistic expectations and frustrate patients.
Tablet-based screening is promising because it is less labor intensive than in-person screening, is acceptable to patients, and is linked to higher disclosure rates across multiple sensitive domains, presumably because social desirability bias is minimized.
[..] We recommend that organizations use a standardized approach — i.e., a single tablet-based screening application and playbook for follow-up conversations — across the institution. We also recommend a flexibly designed survey, such as the Patient-Reported Outcomes Quality of Life (PROQoL) tool, developed by Ridgeway and colleagues. The PROQoL asks patients for their “single biggest concern” at the time of the appointment and focuses screening questions on that topic. Thus, even if multiple departments offer screening, patients need not repeat their responses to questions that they have previously answered, allowing the focus to shift to areas of current concern.
[..] theoretical limitations of the “screen and refer” approach. One possibility is that these programs are often light-touch interventions that provide mostly informational, rather than instrumental, support. Fiori et al. demonstrated an association between more robust support (i.e., more than four outreach encounters, more than 30 days of follow-up) and successful screening and referral of patients to social services.
[..] existing “screen and refer” platforms are seldom informed by the important complexities of social or behavioral science theory.
[..] In contrast, the health system–based social interventions that have been clinical trial–proven to improve health outcomes are typically theory-based programs that provide longitudinal, tailored support [see table below].

[..] IMPaCT, an intensive community health worker intervention for addressing social needs, has been tested in three randomized controlled trials, with rigorous analysis demonstrating that the program reduces total hospital days by 65% and returns $2.47 for every dollar invested by Medicaid. IMPaCT also has been shown to improve mental health, chronic disease control, and quality of care. CareMore’s complex care management program in Memphis, Tennessee, which matched high-need, high-cost Medicaid patients with a care team consisting of a community health worker, a social worker, and the patient’s primary care provider, reduced total medical expenditures by 37% (absolute reduction, $7,732 per member per year) and inpatient utilization by 59%. While these interventions are by no means inexpensive, when they generate thousands of dollars in savings, they pay for themselves.”
Screening for Unmet Social Needs: Patient Engagement or Alienation? Butler ED, Morgan AU and Kangovi S. NEJM Catalyst Innovations in Care Delivery 2020.7.20
“Six months into this pandemic, Americans still dramatically misunderstand the risk of dying from COVID-19:
1.On average, Americans believe that people aged 55 and older account for just over half of total COVID-19 deaths; the actual figure is 92%.
2.Americans believe that people aged 44 and younger account for about 30% of total deaths; the actual figure is 2.7%.
3.Americans overestimate the risk of death from COVID-19 for people aged 24 and younger by a factor of 50; and they think the risk for people aged 65 and older is half of what it actually is (40% vs 80%).
[..] how can there be still such a widespread, fundamental misunderstanding of the basic facts? Our poll results identify two major culprits: the quality of information and the extreme politicization of the COVID-19 debate:
•People who get their information predominantly from social media have the most erroneous and distorted perception of risk.
•Those who identify as Democrats tend to mistakenly overstate the risk of death from COVID-19 for younger people much more than Republicans.
[..] Fear and anger are the most reliable drivers of engagement; scary tales of young victims of the pandemic, intimating that we are all at risk of dying, quickly go viral; so do stories that blame everything on your political adversaries. Both social and traditional media have been churning out both types of narratives in order to generate more clicks and increase their audience.
[..] Our susceptibility to how the information is presented also plays a role. The same data can be portrayed in different forms on a graph—some reassuring and some alarming. Our study finds that how the data are presented has a very strong impact on people’s attitudes. For example, respondents who were shown COVID-19 case trends for Texas and Florida in isolation were much less willing to reopen schools and businesses than those who were shown the same trends compared to New York. And more alarming graphics tend to be used more frequently, as they generate greater engagement.
[..] Individual risk from COVID-19 depends on age and health, but perceived risk depends on one’s politics— and it’s perceived risk that drives behavior.
[..] The policy decision of what activities to keep shut and for how long is a very difficult and consequential one. It requires balancing two opposite effects of uncertain scale: on the one hand the benefits in terms of slowing COVID-19 contagion, on the other hand the harm to the economy and to people’s long-term health and livelihoods. This decision is strongly influenced by public perceptions of dangers, not only because politicians are sensitive to the public’s concerns but also because politicians are people too, subject to some of the same biases. Our poll results suggest fundamental misperceptions of the risk of death or serious adverse health consequences from COVID-19 could be distorting these decisions.”
An initial review of the Franklin Templeton-Gallup Economics of Recovery Study
On My Mind: They Blinded Us From Science, Desai S. Franklin Templeton 2020.7.29
2020.8.19
“Healthy People 2030 features 355 core – or measurable – objectives with 10-year targets, new objectives related to opioid use disorder and youth e-cigarette use, and resources for adapting Healthy People 2030 to emerging public health threats like COVID-19. For the first time, Healthy People 2030 also sets 10-year targets for objectives related to social determinants of health.
[..] A federal advisory committee of 13 external thought leaders and a workgroup of subject matter experts from more than 20 federal agencies contributed to Healthy People 2030, along with public comments received throughout the development process.
The HHS Office of Disease Prevention and Health Promotion leads Healthy People in partnership with the National Center for Health Statistics at the Centers for Disease Control and Prevention, which oversees data in support of the initiative.”
Healthy People 2030 divides objectives into core (measurable) objectives, developmental objectives (evidence-based interventions exist, but no reliable baseline data) and research objectives (high health or economic burden or significant disparities between population groups, but no evidence-based interventions).
The objectives fall into the following categories and subcategories:
HHS Releases Healthy People 2030 with National Disease Prevention and Health Promotion Objectives for the Next Decade, Health & Human Services Press Office, 2020.8.18
“Deep Learning (DL) image reconstruction has the potential to disrupt the current state of MR [magnetic resonance] imaging by significantly decreasing the time required for MR exams. Our goal was to use DL to accelerate MR imaging in order to allow a 5-minute comprehensive examination of the knee, without compromising image quality or diagnostic accuracy. Our goal was to use DL to accelerate MR imaging in order to allow a 5-minute comprehensive examination of the knee, without compromising image quality or diagnostic accuracy.
Methods: A DL model for image reconstruction using a variational network was optimized. The model was trained using dedicated multi-sequence training, in which a single reconstruction model was trained with data from multiple sequences with different contrast and orientations. Following training, data from 108 patients were retrospectively undersampled in a manner that would correspond with a net 3.49-fold acceleration of fully-sampled data acquisition and 1.88-fold acceleration compared to our standard two-fold accelerated parallel acquisition. An interchangeability study was performed, in which the ability of 6 readers to detect internal derangement of the knee was compared for the clinical and DL-accelerated images.
Results: The study demonstrated a high degree of interchangeability between standard and DL-accelerated images. In particular, results showed that interchanging the sequences would result in discordant clinical opinions no more than 4% of the time for any feature evaluated. Moreover, the accelerated sequence was judged by all six readers to have better quality than the clinical sequence.”
NYU researchers have been working with Facebook artificial intelligence experts for two years as part of their fastMRI initiative. In this study, the researchers used 75% less of the raw imaging data acquired to reduce the total time spent in the machine. The image quality appears to be nearly equivalent and radiologists like the new images.
Using Deep Learning to Accelerate Knee MRI at 3T: Results of an Interchangeability Study, Recht MP, Zbontar J, Sodickson DK et al. American Journal of Roentgenology, 2020.6.8
2020.8.18
“Intravenous medicines are complex to prepare and more prone to error, with 35%–48% of intravenous doses erroneous in some way.
[..] Our aim was to investigate the effectiveness of user-testing of medicines guidelines for reducing medication errors. We selected the administration of intravenous medicines by hospital nurses using the UK’s National Health Service (NHS) Injectable Medicines Guide (IMG), due to the increased risk of medication errors with this route of administration. [..] a recent user-testing study identified that in 36 of 340 cases, nurses were unable to find or understand important information in the current IMG. After user-testing, numerous revisions were made to the guidelines, including provision of equations and tables to support dose, dilution and infusion rate calculations, additional subsections, and clearer wording and formatting. Following these changes, the number of instances of nurses being unable to find or understand important information decreased to 3 of 340 cases. Therefore, the specific objective of the present study was to compare the frequency of medication errors made by nurses using current and user-tested IMG guidelines during the preparation and administration of an intravenous medicine.
[..] Participants prepared and administered a simulated intravenous infusion of voriconazole, with observation used to identify medication errors. In situ simulation involves a simulated episode of patient care integrated into the clinical environment with participants who are on-duty health professionals.
[..] In total, 273 participants completed the simulation before recruitment ended with all willing participants recruited and the minimum sample size achieved.
[..] In total, 1504 errors were observed and 267 of 273 simulations (98%) included at least one error of any type. For the primary outcome, although a smaller proportion of the simulations with the user-tested guidelines (49%) included at least one moderate-severe IMG-related error than with the current guidelines (59%), the risk ratio of 0.82 (95% CI 0.66 to 1.02) did not indicate a significant difference. However, the proportion of user-tested guideline simulations without any IMG-related errors (48%) was significantly greater than with the current guidelines (20%), with a risk ratio of 2.46 (95% CI 1.68 to 3.60). This indicates that when using the user-tested guidelines, a simulation was more than twice as likely to have no IMG-related errors than when using the current guidelines. Risk ratios indicate no significant differences between the groups for non-IMG-related errors.
[..] Median completion time for the simulation was 1.6 min (95% CI 0.2 to 3.0) faster with the user-tested guidelines, indicating a statistically significant decrease in completion time. There was a statistically significant 45% increase in the chance of completing the simulation if using the user-tested guidelines compared with the current guidelines (HR 1.45, 95% CI 1.11 to 1.89). [..] After comparing both versions of the guidelines, 129 participants allocated the current guidelines (97%) and 122 participants allocated the user-tested guidelines (87%) expressed at least some preference for the user-tested guidelines.
[..] The guideline revisions likely to have contributed to the reduced frequency of errors after user-testing can be identified by considering the error types with the largest reduction. These include dose and rate discrepancies (including administration by short injection rather than infusion), suggesting that the improved support for dose, rate and dilution calculations in the user-tested guidelines (eg, equations and tables) at least partially contributed to safer and faster preparation and administration of the medicine. This is consistent with the findings of our previous study, where dose and rate calculation problems occurred more often with the current guidelines than with the user-tested guidelines. A common calculation error with the current guidelines was not accounting for displacement volume when measuring the volume of drug solution containing the prescribed dose. The user-tested guidelines helped prevent this error by providing an equation for this calculation. A common rate discrepancy with the current guidelines was to administer the infusion over 1 hour. The instructions stated ‘give over 1–3 hours (maximum rate 3 mg/kg/hour)’, and some participants used the first time listed (1 hour) rather than calculating the maximum infusion rate based on the second part of this instruction (3 mg/kg/hour=2 hours). The user-tested guidelines did not present this range of infusion times (which was only applicable to some doses) and instead provided a table of infusion lengths and an equation to support the calculation, thus preventing this error. This suggests that guideline authors should provide equations and tables to support health professionals making calculations. However, as different ways of presenting information may be successful in different contexts, the safety improvements suggested by this study will be best achieved through user-testing.”
User-testing guidelines to improve the safety of intravenous medicines administration: a randomised in situ simulation study, Jones MD, McGrogan A, Raynor DK M et al. BMJ Quality & Safety 2020.6.30
“Poor dietary quality has surpassed all other mortality risk factors, accounting for 11 million deaths and ≈50% of cardiovascular disease (CVD) deaths globally. Paralleling this trend, US healthcare expenditures have grown steadily and now represent 17.9% of the gross domestic product in 2016, nearly half of which was accounted for by obesity-related conditions ($1.42 trillion/y). Dietary interventions focused on single nutrients (eg, vitamin D, omega-3 fatty acids) have not adequately reduced incident CVD. Conversely, dietary patterns low in fruits, vegetables, and whole grains and high in red and processed meat, added sugars, sodium, and total energy are the leading determinants of CVD, Alzheimer disease, some cancers, and diabetes mellitus risks. As a result, strategies that promote holistically healthier dietary patterns to reduce chronic disease risk are of contemporary importance.
[..] Once diet is assessed, CDS [clinical decision support] can help clinicians and other members of the healthcare team engage patients in diet education and evidence-based behavior counseling. For instance, a systematic review conducted by the US Preventive Services Task Force found that in adults not at high risk for CVD, behavioral counseling for diet and physical activity resulted in modest benefits in blood pressure, low-density lipoprotein and total cholesterol levels, and body weight, resulting in a US Preventive Services Task Force C recommendation for a positive but small benefit.
[..] national data have shown that US adults 20 to 65 years of age have suboptimal diet quality, achieving 60% to 65% of ideal scores. Although diet quality is positively correlated with socioeconomic indicators, low nutrition knowledge was associated with low diet quality regardless of education and income.
[..] Even brief diet counseling led to a significant, albeit modest, improvement in diet quality, as well as body weight, total cholesterol, low-density lipoprotein cholesterol and fasting glucose concentrations, systolic and diastolic blood pressures, and incident diabetes mellitus. Limited evidence demonstrated that intensive counseling involving registered dietitians increased dietary quality by increasing the intake of fruits, vegetables, and nuts and decreasing the intake of commercial baked goods.
[..] Of the 15 tools reviewed for this statement, the 3 that met the greatest number of theoretical and practice based
validity criteria were the Mediterranean Diet Adherence Screener (MEDAS) and its variations, the modified, shortened Rapid Eating Assessment for Participants (REAP), and the modified version of the previously validated Starting the Conversation tool. Although the Starting the Conversation tool met 0.5 fewer criteria than the PrimeScreen tool, we chose to discuss it given its frequency of use in clinical practice.”

Rapid Diet Assessment Screening Tools for Cardiovascular Disease Risk Reduction Across Healthcare Settings: A Scientific Statement From the American Heart Association, American Heart Association Council on Lifestyle and Metabolic Health; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; Council on Stroke Cardiology; and Stroke Council. Circulation: Cardiovascular Quality and Outcomes, 2020.8.7
“The 20-m shuttle run test (20mSRT) and its variants are now the most widely used tests to estimate CRF in youth in the world. [..] Typically, youth are instructed to run at an increasing standardized pace (starting at ≈5 mph [8 km/h], increasing in 0.3-mph [0.5-km/h] increments each minute), noting the number of laps or stages during which they can keep up with the pace, which can then be compared with results from a reference population.
[..] In the United States, the 20mSRT is commonly used as a component in the FITNESSGRAM. The FITNESSGRAM is a group of tests used to assess various forms of fitness in school-aged youth. In addition to the 20mSRT, the FITNESSGRAM measures body mass index (BMI), abdominal strength, trunk extensor strength, upper-body strength, and flexibility. The results are classified into various fitness zones. All 50 states in the United States currently use the FITNESSGRAM to assess >22 million students each year. [The FITNESSGRAM is managed by the Cooper Institute that charges a fee to access their tools.]
[..] In terms of the validity of the 1.5-mile and 12-minute run tests compared with the similarly reliable 20mSRT, data from 2 large meta-analyses indicate that run tests are equally valid compared with the 20mSRT.
[..] The pecentage of boys [in the United States] who had healthy CRF [cardiorespiratory fitness] decreased significantly from 65% in 1999 to 2000 to 50% in 2012. For girls, the percentage decreased over the same time period, although not as substantially, from 41% to 34%. In addition, 54% of normal-weight youth had healthy CRF, whereas only 30% of youth who were overweight (BMI ≥85th percentile for age and sex) and 20% of youth with obesity (BMI ≥95th percentile for age and sex) had healthy CRF. This percentage did not differ by race and Hispanic origin or ratio of family income to poverty.
[..] Every child will benefit from a CRF estimate as part of a yearly physical. Repeated bursts of vigorous physical activity, including HIIT, improve youth CRF. Public health measures and school policies that support lifestyle improvements to improve CRF in individuals and populations are expected to result in substantial health and cognitive benefits.”
The authors acknowledge that cardiorespiratory fitness is only one of four distinct health-related fitness components (the others are muscular fitness, flexibility and body composition).
Cardiorespiratory fitness in youth: an important marker of health: a scientific statement from the American Heart Association, American Heart Association Young Hearts Athero, Hypertension and Obesity in the Young Committee of the Council on Lifelong Congenital Heart Disease and Heart Health in the Young. Circulation, 2020.8.18
2020.8.13
“The coronavirus pandemic has strained health systems, revealed unconscionable inequalities, and upended international institutions. Here are 7 critical lessons.
- Build resilient health systems – [..] core health system capacities, including surveillance, laboratories, human resources, and risk communication. Health systems also need capacity to test for, diagnose and treat infectious diseases. [..] Resilient health systems require surge capacity to cope with health emergencies in the event hospitals become overrun.
- Leadership and public trust are the single greatest indicator of success – [..] Perhaps the single greatest indicator of success in responding to COVID-19 has been whether governments gain the public’s trust. Population-based health behaviors—handwashing and other aspects of personal hygiene, physical distancing, and face coverings—can significantly reduce community spread.
- Defend the integrity of science and public health agencies – [..] Within weeks of reports of a cluster of atypical pneumonia cases in Wuhan, China, scientists had sequenced the virus. Epidemiological studies subsequently determined severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was transmitted person to person, including by asymptomatic individuals. Further research showed that personal hygiene, physical distancing, and face coverings were effective nontherapeutic interventions. Research laboratories rapidly developed viral and antibody testing technologies. There is promising scientific research into effective vaccines and therapeutics. Within 6 months, 6 vaccine candidates were in phase 3 clinical trials. Despite remarkable, albeit incomplete, scientific discovery, populist political leaders have sown doubt about the value of science and have undermined public health agencies. In Brazil and the US, for example, political leaders have publicly recommended COVID-19 treatments that their own agencies have not approved, such as hydroxychloroquine. President Trump publicly criticized US Centers for Disease Control and Prevention guidelines for reopening schools. If political leaders fail to implement evidence-based policies or to convey consistent messages based on science, the COVID-19 response will be suboptimal.
- Invest in biomedical research and development – [..] Governments must sustainably invest in biomedical research and development, not just during a health crisis but also during interpandemic periods. After the West Africa Ebola epidemic, the Commission on a Global Health Risk Framework for the Future recommended an incremental increase of $1 billion per year to accelerate research and development for innovative medical technologies. Even $1 billion annually is far too low given the economic devastation of the pandemic, with the World Bank projecting a 5.2% contraction in global GDP in 2020.
- Focus on equity: the prevailing narrative of this age – Even before the coronavirus pandemic, social, economic, and health inequities became the prevailing global narrative. Yet, COVID-19 amplified long-standing systemic inequalities, including access to health care. SARS-CoV-2 infections and COVID-19 deaths disproportionately affected racial minorities including Black, Hispanic, and Native American individuals. Many lower-paid workers, such as those in grocery stores, meatpacking plants, and truck drivers, were exposed to individuals with SARS-CoV-2 infection. [..] Populations everywhere are expressing anger with enduring health, social, and economic injustices.
- Adopt evidence-based laws: safeguard the rule of law – [..] The US Supreme Court has ruled on COVID-19–related cases in relation to voting and religious freedom, but it has not yet opined on the liberty-limiting regulations imposed during the COVID-19 response. Responding to expansions of political power in countries like Russia, Turkey, and Hungary, the United Nations launched a Rule of Law project on COVID-19. Emergency health powers should be based on evidence and used only when there are no less restrictive alternatives. Usurpation of power under the pretext of a health crisis threatens to erode democratic freedoms, which can endure even after the crisis ends.
- Fund and support robust global institutions: we are in this together – [..] Public and private partners joined with the WHO to launch the Access to COVID-19 Tools (ACT) Accelerator, a global collaboration to accelerate research and development, production, and equitable access to COVID-19 tests, treatments, and vaccines. COVAX—a partnership between Gavi, the Coalition for Epidemic Preparedness Innovations, and the WHO—is the vaccine arm of ACT, designed to facilitate the discovery of COVID-19 vaccines and guarantee fair and equitable global access.”
The Great Coronavirus Pandemic of 2020—7 Critical Lessons, Gostin LO. JAMA Health Forum 2020.8.13
Excerpt – [UT Austin Department of Surgery Chair and orthopedic surgeon Kevin] Bozic adds. “I would argue that the problem is not access to care, the problem is not the cost of care, and the problem is not variability and the quality of outputs. The problem is that health care often doesn’t produce more health. As my colleague Scott Wallace from our Value Institute for Health & Care at UT Austin has taught me: If health is not improved, then value is zero.”
“We’ve now had about a decade of experience evaluating the impact of the bundled payment models on patient outcomes and costs, and I can summarize that and tell you that the overall result has been a slight reduction in the episode cost of care with no detrimental impact on patient outcomes. [..]”
“It’s never made sense to me why, if you had knee pain, you would see an orthopedic surgeon; but I have patients all the time who come to me with knee pain,” Bozic says. “If I have a headache, I don’t call a neurosurgeon. That’s not the first place I go, but a patient with knee pain sees an orthopedic surgeon.”
Instead, we should ask these types of questions: “What do we need to do to care for patients with musculoskeletal pain? What are the different services that we need to provide and what’s the multidisciplinary team we’d need to put together that’s focused on the outcomes that matter to those patients?”
“What we learned in that experiment here in Austin is that patient activation is critical. Patient activation is essentially measuring a patient’s propensity to engage in healthy behavior,” Bozic says. “When we saw Ms. Adams, she had a patient activation level of one, which meant she was not confident enough to play an active role in her own health and, therefore, was predisposed to be a passive recipient of care. We know from our own research that leads to poor outcomes with surgical treatment.” [..]
“[..] no one bothered to ask what was important to her and what she was hoping to gain from the treatment in the first place,” Bozic says. “No one asked her about her preferences, values, or expectations, and no one bothered to measure the things that matter most to her, which were pain, functional status, and quality of life.”
Bozic’s group applies predictable analytic tools to help patients and their clinical teams make shared, informed decisions about treatment based on their individual circumstances. “Turns out we can identify from a patient’s baseline pain, physical function, and mental health their likelihood of improving from surgery,” Bozic says. “If Ms. Adams had had access to this type of tool, she’d have realized that she had less than a 50% chance of reducing her pain and improving her function with surgery because, as I explain to all of my patients, the biggest risk of surgery is not developing a blood clot or having an infection or even death; the biggest risk is undergoing a major surgical procedure and not improving your health.”
Innovation Must Include Patient Preference and Activation Measures, Bozic K. NEJM Catalyst Innovations in Care Delivery, 2020.7.27
2020.8.12
“The Administration’s surprise billing principles include:
- Patients receiving emergency care should not be forced to shoulder extra costs billed by a care provider but not covered by their insurer.
- Patients receiving scheduled care should have information about whether providers are in or out of their network and what costs they may face.
- Patients should not receive surprise bills from out-of-network providers they did not choose and
- Federal healthcare expenditures should not increase.
[..] Surprise billing most often involves a facility’s “ancillary” providers, that is, a hospital’s emergency medicine personnel, anesthesiologists, pathologists, radiologists and neonatologists, as well as assistant surgeons, hospitalists and intensivists.
[..] Hospitals are increasingly relying on third party staffing firms to meet their needs for personnel, which is contributing to surprise billing. These private staffing firms are often used to staff emergency rooms and to provide specialty care in areas such as anesthesiology, gastroenterology, urology and orthopedics.
[..] Private equity plays a large role in third party staffing: the two largest physician staffing firms, Envision/EmCare and TeamHealth, are each owned by private equity firms. Research shows that when private equity firms enter a market the rate of out-of-network billing increases by large percentages: 66 percent for Envision/EmCare and 13 percent for TeamHealth.
[..] Surprise billing in private health insurance represents a market failure that will not correct itself. It is rooted in the complex web of contractual arrangements between patients, employers who sponsor health plans, and health plans and their provider networks and the contractual arrangements between these parties within a network-based service delivery model. For surprise bills associated with emergency care, the patient generally has neither the information nor the option to seek care elsewhere and should be protected from abnormally higher out-of-network prices. For surprise bills associated with scheduled procedures, the patient usually lacks information about the use of out-of-network ancillary providers and generally does not have the opportunity to weigh options or provide informed consent, or they may be faced with these decisions while already in the process of receiving care. [..] Currently, in too many cases, consumers are left to make decisions with incomplete information about the network status of providers and the estimated costs of care and are caught between provider and payer, neither of which have sufficient incentive to protect the consumer. Basic consumer protections that provide cost transparency, informed consent, and anti-price gouging should also apply to the uninsured.
[..] The legislation of 15 states meet criteria that researchers at Georgetown have identified as comprehensive. That is, they:
- Extend protections to both emergency and non-emergency services;
- Apply balance billing laws to all types of insurance that are subject to state regulation, including Health Maintenance Organizations and Preferred Provider Organizations;
- Protect consumers both by requiring that insurers hold them harmless from extra provider charges – meaning they are not responsible for the charges – and by prohibiting providers from balance billing; and
- Adopt an adequate payment standard – a rule to determine how much the insurer pays the
provider – or an arbitration process to resolve payment disputes between providers and insurers.
In order to effectively address surprise billing, federal legislation is needed to address all ERISA group health plans, including self-insured ERISA arrangements that state legislation cannot address, and to provide a national surprise billing standard that would apply to all states. Legislation needs to be simple and fair for patients and not place implementation barriers on health plans, insurers, and providers.”
The manuscript includes a description of New York’s experience after passing suprise billing legislation in 2014 (going into effect early 2015).
“New York uses an independent dispute resolution (IDR) process for resolving disputes between providers and health insurance issuers. Each party makes its best offer and an IDR entity decides which is the most “reasonable.” The state’s guidance provides that arbiters should consider the 80th percentile of all charges for the particular health care service performed by a provider in the same or similar specialty and provided in the same geographical area as reported in a benchmarking database in determining payment.
The state of New York issued a report on its surprise billing law finding that the law has saved consumers over $400,000,000 in emergency room services between March 2015 and the end of 2018. The report also cites a separate paper’s findings that through 2015 the New York law reduced out-of-network billing by 34 percent and lowered in-network emergency physician payments by 9 percent. For the years 2015 through 2018, the report found that 43 percent of emergency services IDR results were in favor of the health plan, 24 percent were in favor of the provider, and 33 percent were split between both parties. The specialties most often involved in IDR decisions not involving emergency services were neurosurgery (31 percent of IDR disputes) anesthesiology (25 percent), plastic surgery (15 percent) and neurology (12 percent). [..]
While New York asserts consumer savings from its legislation, researchers at the Brookings Institute suggest that the state’s IDR process is increasing health care costs by having the arbiters consider the 80th percentile of billed charges when determining payment in a dispute. Charges are typically much higher than negotiated network rates. Moreover, Brookings has found that New York arbitration decisions have averaged 8 percent higher than the 80th percentile of charges. Brookings also finds that when the insurer “wins,” its payment averages only 11 percent below the 80th percentile of charges, far above negotiated rates, implying the process is increasing, not decreasing costs.”
HHS Secretary’s Report on: Addressing Surprise Medical Biling: July 2020, US Department of Health & Human Services Office of the Assistant Secretary for Planning and Evaluation
“One way of answering this question is to assess why we spend so much more than other countries do.
[..] The first problem with these analyses is that as nations and people grow richer, they’re willing to spend a greater share of income on health care. The fact that U.S. incomes are nearly 25% higher than U.K. incomes, for example, suggests that we would be spending 15 to 25% more on health care, all else being equal (the same point highlights the challenges of putting all Americans, with very disparate incomes, into a single insurance plan).
Second, our measures of quantity don’t adequately capture the quality or intensity of care, misleadingly suggesting that spending differences must be attributable to price when there are probably unmeasured differences in quality or intensity that masquerade as higher prices. [..] The question ought to be whether the expenditures on greater quality or intensity, appearing as higher prices, are generating care improvements of sufficient value — a very different exercise from taking on prices alone.
The third problem with these comparisons is that prices, quantities, and quality affect one another, so they aren’t independent policy levers: a change in prices would also change the quantity and quality of care. Knowing whether prices are “too high” hinges on understanding the forces that determine these prices and on whether lower prices would result in desirable or undesirable changes in the care delivered. For example, high prices that result from anticompetitive mergers suggest different policy reactions than high prices that result from patients choosing more expensive providers over less expensive ones: for patients, 10% higher perceived quality might be worth paying 30% more. If prices truly reflect patient demand for valued care, then administratively setting lower prices may harm patients. Furthermore, administratively setting prices below market levels risks achieving short-term savings at the cost of reducing valuable long-run innovations. Similarly, most health care spending is on labor, and wages depend on forces outside health care (such as the wages aspiring physicians would be paid if they chose to be lawyers instead); regulation thus has limited power to lower prices without generating offsetting quality effects.
A better way to determine whether we spend too much on health care is to assess our health outcomes relative to how much was spent to achieve them — to see how much health benefit we get for every dollar spent. There’s evidence that we overspend on some kinds of care and underspend on others, including prevention, vaccines, and basic care for the uninsured. High-value care doesn’t mean cheap care, and low-value care doesn’t mean expensive care: some expensive treatments generate enormous value, such as cures for hepatitis C and rapid stenting after a heart attack; and some low-cost care is wasteful, such as antibiotics for viral infections or annual checkups for well patients. We can’t simply say we spend too much; rather, we’re not spending on consistently high-value care.
[..] Moving to higher-value care is much harder than reducing spending, because it requires spending more on certain types of care while saying no to things that improve health at a cost that’s too high.
Promises of reforms that will both reduce spending and improve outcomes are popular to make, but evidence (and Congressional Budget Office scoring) suggests that they’re difficult to keep. Most preventive care improves health but doesn’t save money. Health insurance expansions improve financial security and health but increase spending. Paying primary care physicians to coordinate care across settings or “hot-spotting” programs that target patients with high health care use may improve the quality of care but don’t reduce spending.
[..] The debate about whether health care is a right sidesteps the more difficult and important question of how much health care is a right that should be ensured through public programs.
There are multiple drivers of the quantity and value of health care delivered — and thus opportunities for innovation. The way health care is paid for highlights the misalignment of incentives to assess value within health care and relative to other priorities. Medicaid, jointly financed by the states and the federal government, is constrained by states’ ability to borrow. [..] Medicare, financed by the federal government, can operate at a deficit for longer — but has limited tools for moving toward paying for value. It’s prohibited from using cost-effectiveness in coverage decisions, and although fee-for-service payment is not the only culprit, Medicare’s limited alternative payment schemes suffer from weak incentives and inadequate measurement. Moreover, Medicare has outsized effects on coverage and spending throughout the health care system, given its size and the precedent it sets for private insurers, infrastructure investment, and incentives for innovation.
Coverage by employer-sponsored insurance plans is shaped by the wages that employees are willing to give up for their health insurance benefit, but this trade-off is further distorted by the tax-subsidizing of generous plans (with greater subsidies for higher-income workers), which drives more of workers’ compensation toward richer insurance benefits that cater to higher-income employees. Reducing this regressive tax subsidy would greatly improve both equity and the value of care, but it has proven politically fraught. On the patient side, cost sharing is often misperceived as merely a mechanism for shifting costs to enrollees, but it can help limit the use of low-value services. Crude cost-sharing implementations, such as across-the-board high deductibles or copayments, however, can discourage high-value as much as low-value spending.
Thus, the options available to policymakers must be assessed on the basis of their effects on both spending and health outcomes. Higher payments for high-value services may spur innovations that improve the length and quality of life. But these advances bring tough choices, and a one-size-fits-all solution probably can’t both achieve public policy goals and meet individual priorities. There is a strong rationale for public plans to ensure that all people have access to highly beneficial care, regardless of their ability to pay. Public programs could cover many more people if their resources were focused on high-value care, rather than on covering all services for fewer people. But many people may be willing to pay more for innovations even of limited or uncertain health benefit, and insurers can tailor plans to generate value to attract enrollees. If we’re willing to pay $150,000 for each quality-adjusted extra year of life (a commonly used estimate), then we ought to view a 10% increase in spending per capita as a good investment if it extended average life expectancy by 2.5 days. That number may give readers pause — hence the importance of clarifying our spending priorities and focusing on care that produces real value for patients. With such a focus, we could feel more confident that higher health care spending was worth it.”
Do We Spend Too Much on Health Care? Baicker K and Chandra A. NEJM 2020.8.13
“given that routine physical examinations have been shown to have limited clinical value, we believe health care organizations should take this opportunity to advance alternative systems for promoting evidence-based prevention. Failure to do so will sustain or worsen the long-standing disparities in health that have been underscored by the pandemic.
[..] We believe the U.S. health care system should embrace this moment as an opportunity to shift the locus of preventive care from face-to-face annual exams to a strategy that focuses on population health: clinical registries that readily identify all preventive services for which a patient is due; annual prevention kits for patients that facilitate widespread deployment of home-based testing, shared decision making, and self-scheduling of preventive screening tests and procedures in more convenient and approachable community settings; and robust community-based strategies involving navigators to overcome health disparities in underserved populations.
The first step in this strategy is developing a robust, real-time clinical preventive care registry that allows tracking of care needs asynchronously from visits. [..] Although many health systems and EHR [electronic health records] vendors have established registry functionality, there is a pressing need for “smarter” registries that are interoperable across diverse health care settings, regardless of EHR vendor, and that can analyze utilization patterns, health conditions, and demographics to help link patients to the best prevention approach for them. These registries could also become shared, interactive tools for use by both clinicians and patients to facilitate preventive care.
The second step is to build the infrastructure for an annual “prevention kit” received by every patient. The kit should consist of a language-appropriate, culturally sensitive package that addresses all indicated USPSTF [US Preventive Services Task Force] grade A and B preventive services as indicated by the clinical prevention registry. Point-of-care tests should be included to allow preventive care to happen from patients’ homes; these could include fecal immunochemical testing, glycated hemoglobin and lipid testing, and perhaps soon, self-sampling of human papilloma virus for cervical cancer screening. QR code links to standardized electronic questionnaires should be included for depression screening, tobacco and alcohol use, and personalized risk assessment for common conditions such as breast cancer and cardiovascular disease. Shared-decision-making materials for lung cancer screening, breast cancer screening intervals, and highly controversial topics such as prostate cancer screening are well studied and easily deployed. Self-scheduling instructions for all recommended procedures and imaging studies should be provided.
After receiving the prevention kit, patients could be invited to schedule a virtual encounter with their primary care provider to review recommendations, engage in shared decision making on nuanced topics such as when to start or stop each type of screening, discuss any findings that may be of concern, and plan necessary interventions. Immunizations and other high-value preventive care that cannot be delivered at home could be addressed during in-person patient visits or at dedicated immunization clinics, rather than during dedicated annual exams.
The third step is to create specific programs to address the known disparities in preventive care within a given population. There is a rich body of literature supporting the effectiveness of community-based patient navigators in closing gaps in cancer-screening rates affecting underserved patients. These navigators facilitate patients’ preventive care by using proactive outreach and motivational interviewing and by accompanying patients to procedures such as colonoscopies. Navigators are also well suited to systematically screening for and facilitating access to community-based resources for addressing social determinants of health. In addition, they can connect patients with community-based campaigns to promote prevention, such as screening vans. Though navigation programs cannot eliminate key social determinants of poor health, such as poverty, educational barriers, food insecurity, and racism, they can help make access to evidence-based preventive services more equitable.
[..] Both patients and clinicians will have discovered virtual visits’ potential for discussion and counseling. If we move to more sophisticated systems that can deliver convenient, personalized home-based testing strategies to patients, engage patients in their own care, and deploy evidence-based programs to ensure equitable access to preventive services, we believe our population’s health will be improved.”
Covid-19 and the Mandate to Redefine Preventive Care, Horn DM and Haas JS. NEJM, 2020.8.12
A few of the Office of Inspector General’s top unimplemented recommendations from audits and evaluations issued through December 31, 2019:
Centers for Medicare & Medicaid Services (CMS)―Medicare Parts A and B
- CMS should take actions to ensure that incidents of potential abuse or neglect of Medicare
beneficiaries are identified and reported. - CMS should reevaluate the inpatient rehabilitation facility payment system, which could include
seeking legislative authority to make any changes necessary to more closely align inpatient rehabilitation facility payment rates and costs. - CMS should seek legislative authority to comprehensively reform the hospital wage index system.
- CMS should seek legislative authority to implement least costly alternative policies for Part B drugs
under appropriate circumstances. - CMS should provide consumers with additional information about hospices’ performance via Hospice Compare.
- CMS should continue to work with the Accredited Standards Committee X12 to ensure that medical device-specific information is included on claim forms and require hospitals to use certain condition codes for reporting device replacement procedures.
- CMS should analyze the potential impacts of counting time spent as an outpatient toward the 3-night requirement for skilled nursing facility (SNF) services so that beneficiaries receiving similar hospital care have similar access to these services.
CMS―Medicare Parts C and D
- CMS should provide targeted oversight of Medicare Advantage organizations (MAOs) that had risk adjusted payments resulting from unlinked chart reviews for beneficiaries who had no service records in the 2016 encounter data.
- CMS should require MAOs to submit ordering and referring provider identifiers for applicable records in the encounter data.
- CMS should develop and execute a strategy to ensure that Part D does not pay for drugs that should be
covered by the Part A hospice benefit.
CMS―Medicaid
- CMS should ensure that States’ reporting of national Medicaid data is complete, accurate, and timely.
- CMS should collaborate with partners to develop strategies for improving rates of followup care for children treated for attention deficit hyperactivity disorder (ADHD).
- CMS should develop policies and procedures to improve the timeliness of recovering Medicaid overpayments and recover uncollected amounts identified by OIG’s audits.
- CMS should identify States that have limited availability of behavioral health services and develop strategies and share information to ensure that Medicaid managed care enrollees have timely access to these services.
General Departmental
- HHS should develop departmentwide objectives and a strategic framework for responding to international public health emergencies.
- HHS should ensure that all future web application developments incorporate security requirements from an industry recognized web application security standard.
- CMS and the Health Resources and Services Administration (HRSA) should ensure that States can pay correctly for 340B-purchased drugs billed to Medicaid, by requiring claim-level methods to identify 340B drugs and sharing the official 340B ceiling prices.
2020 OIG’s Top Unimplemented Recommendations: Solutions to Reduce Fraud, Waste, and Abuse in HHS Programs, US Department of Health and Human Services Office of the Inspector General, August 2020
2020.8.10
“Yet, while the US has played a leadership role so many times in the past, we are at a critical juncture where we also need to heed the lessons learned from others as the US falls further behind in its COVID-19 response. Drawing from our experiences, we put forth seven lessons learned from efforts to protect global health that, if applied here at home, will help to reduce inequities and improve the health of all Americans. [..]
- Refocus on public health
- Address inequity by linking development with health
- Invest in reaching people where they are
- Focus delivery on those most marginalized
- Invest in universal health care
- Make medicines affordable
- Provide effective leadership”
[..] We must apply the same ethos to the shocking underlying disparities that exist in US cities such as Minneapolis/St. Paul. There, 25.4 percent of Black residents live in poverty compared to 5.9 percent of White residents; Black residents are three times less likely to own a home than White residents; and Minnesota is the worst state in the nation for racial disparities in high school graduation—67.4 percent for Black students compared with 88.4 percent for White students. Our social safety nets are beyond frayed, and they are exacerbated by systemic racism. We know that we cannot achieve a healthy America without addressing inequities in people’s basic needs and the roots of their poverty.
[..] US public health leaders could learn a great deal if they sat down with community health workers in rural Malawi. Nationally funded community health teams support pregnant women to receive timely care, locate people who have started but not completed tuberculosis treatment, and ensure care does not stop at the walls of the clinic. The Affordable Care Act made it easier for health systems to engage community health workers, and there are numerous successful examples of their use, especially in chronic disease management. Yet, the US has not fully embraced the concept of community health workers, and there is much more we can do—including helping to fulfill the need for at least 180,000 contact tracers and community support workers to strengthen our response to COVID-19.
[..] in the US, many private health systems and insurers are not incentivized to engage beyond their walls and ensure access to those who most need care. Even as the COVID-19 crisis has resulted in a greater proportion of US hospitals on the brink of insolvency, private health insurers have often had to be cajoled by state officials to pay for telehealth and reduce barriers to access. We need a robust public policy dialogue around the societal expectations of health systems and third-party payers to ensure they play a more effective role in future public health crises.
How Lessons from Global Health Can Improve Health And The Response To COVID-19 In The US, Holmes CB and Goosby EP. Health Affairs blog 2020.8.10
2020.8.8
“Emergency department (ED) utilization has risen in recent years, as has the intensity of care provided in the ED, with more tests and treatments performed during a typical visit. While outcomes have improved for Medicare beneficiaries using the ED, the increased intensity of emergency care has led to greater mean charges per ED visit and greater total spending within the ED.
[..] even in the era of alternative payment models and episodes of care, there is surprisingly little evidence regarding how total costs of an emergency care episode have changed in recent years. Such data are needed to better evaluate whether ED care is generating more value over time or whether greater up-front costs are triggering additional downstream spending and adding to the waste in the health care system.
[..] We included ED visits among a random 5% sample of traditional Medicare beneficiaries in 2009 and 2010 and a 20% sample of traditional Medicare beneficiaries in 2011 to 2016. [..] We identified all claims within 30 and 90 days of the index ED visit for physician services, outpatient services, hospital admissions, and postacute care services (including skilled nursing and home health services).
[..] The analysis was limited to the 40 most frequent diagnosis categories (14,355,661 of 18,614,363 visits [77.1%]). [..] Beneficiaries aged 65 years or older who were continuously enrolled in the traditional fee-for-service model were included.
[..] For visits resulting in discharge from the ED, the index visit cost was calculated using outpatient ED facility claims. For visits resulting in admission, the index cost was defined by the associated inpatient diagnosis-related group payment. For visits resulting in observation, the index cost was calculated by including the outpatient ED facility claim in addition to the costs of any associated observation claims. We chose this approach because the disposition decision made by the emergency physician has substantial implications for clinical outcomes and cost.
[..] After excluding 572,361 visits for missing principal diagnosis codes, there were 14,113,088 ED visits from 2011 to 2016 in our sample at 4730 hospital EDs.

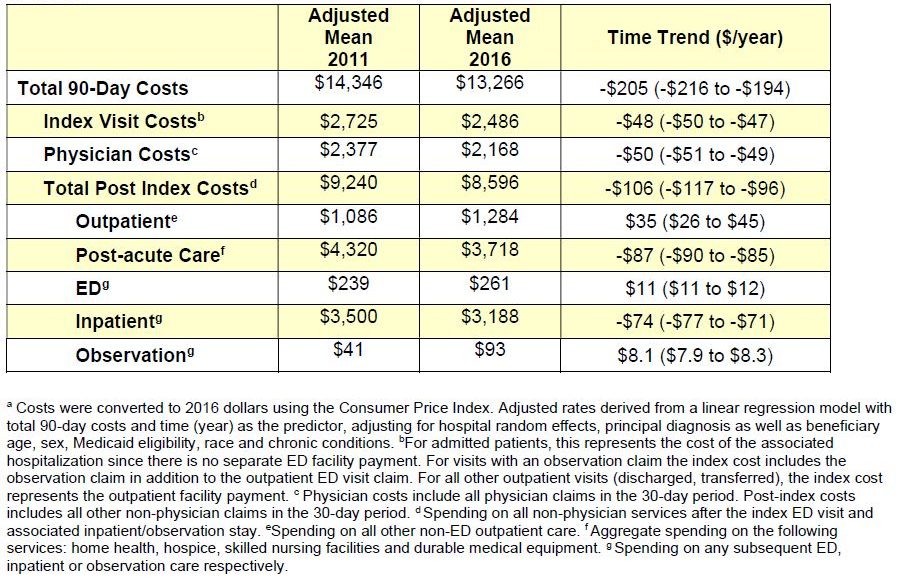
[..] in analyses stratified by disposition, the mean cost per index visit rose within each group. However, total Medicare spending on index ED visits fell over time, as fewer beneficiaries were admitted to the hospital for costly inpatient care at the conclusion of their ED stay. The declines in total costs of care were present across nearly every major diagnosis, although the magnitude of the decline varied by condition.
[..] we found that when we examined all ED visits in aggregate, the total costs of the index visit decreased over time as fewer patients were admitted to the hospital. This decline in up-front costs for ED patients did not lead to a commensurate increase in downstream spending, and on balance, total spending declined over time at 30 and 90 days. While the 8% relative decline in total 30-day costs during the 6-year study period may be considered modest, this represents substantial savings to Medicare and stands in contrast to the overall increase in health care spending more broadly during the same period. Given that mortality has also declined for Medicare beneficiaries using the ED during this period,4 the decline in total spending on ED episodes of care appears not to have occurred at the expense of patient outcomes. However, data using other outcome measures would be helpful to further explore this hypothesis.
[..] while outpatient ED visits are often portrayed as a failure of the primary care system to manage acute and chronic diseases, our results suggest some of the rise in outpatient ED visits may actually reflect the success of the ED in avoiding more costly inpatient care. [..] Regardless of the precise mechanism, our results suggest that a narrow focus on cost trends for ED visits ending in discharge (rather than all visits) may obscure the broader role of the ED in the transition to an outpatient delivery model of acute care.”
Trends in Costs of Care for Medicare Beneficiaries Treated in the Emergency Department From 2011 to 2016, Burke LG, Burke RC, Epstein SK et al. JAMA Network Open 2020.8.6
“Some policy makers believe that expanding the Medicare model, which has a financing system that more closely resembles that of other high-income countries (ie, it is government run and tax financed), could reduce spending substantially. To examine whether this policy has potential, this cross-sectional study compared nominal and relative spending in the US, by 5-year age groupings, with that of other high-income countries that have more homogenous financing systems. This comparison allows us to better understand spending differentials between the US and other countries for people aged 65 years or older, as well as for other age groups.
[..] We used data from the Organisation for Economic Co-operation and Development2 to examine variations in total current health care spending per capita, by age cohort, for the US and 7 other high-income countries (ie, Australia, Canada, Germany, Japan, the Netherlands, Switzerland, and the United Kingdom) in 2015. These data were derived from national sources and the “Health Expenditures by Diseases and Conditions” report. For the US, per capita health spending by age cohort was derived from 2013 Institute for Health Metrics and Evaluation expenditure. Data on the US 2015 population structure were obtained from the United Nations “World Population Prospects: The 2017 Revision.” Expenditure data were translated into US dollar equivalents using 2015 actual individual consumption purchasing power parities from the Organisation for Economic Co-operation and Development.
[..] For all 7 comparator countries, the mean (SD) per capita spending in health care was $4924 ($937). In the US, per capita health care spending was $9524, or 1.9-fold higher than the mean for the 7 comparator countries.
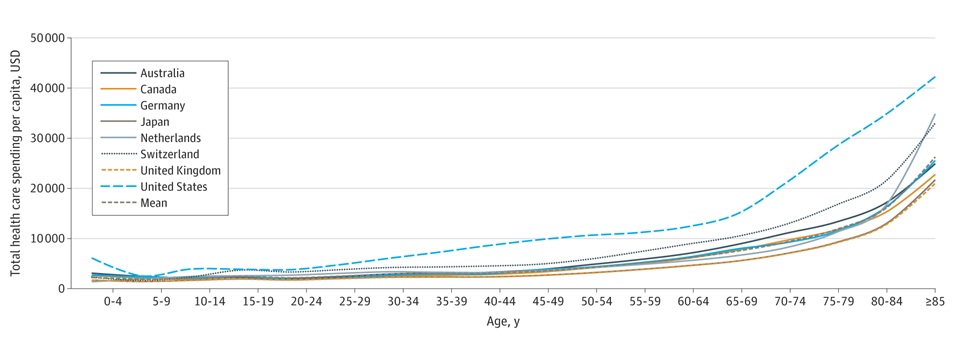

[..] The ratio of spending in the US to that in comparator countries was lower for people aged 65 years and older (2.0-fold the mean) than for those aged 20 to 64 years (2.3-fold). However, the Medicare-eligible population in the US still spent 100% more per capita on health care than older adults spent in the 7 comparator countries. In addition, the narrowing in the spending gap for individuals aged 65 and older was driven by substantial increases in spending among those aged 85 years and older in the comparator nations, not by a reduction in spending in the US older population.
[..] Our findings suggest that despite appearing similar in structure to the health care systems of other high-income countries, the US health care system for individuals aged 65 years and older is comparably more costly. These findings suggest that moving to a Medicare-for-all model may not substantially reduce US health care spending relative to that of other high-income countries.”
Comparison of Health Care Spending by Age in 8 High-Income Countries, Papanicolas I, Marino A, Lorenzoni L and Jha A. JAMA Network Open 2020.8.6
2020.8.5
“over the past decade, health-plan spending for such treatments [specialty drugs] increased from an estimated 26% of total drug spending to 49%, while the treatments remained below 2.5% of total prescriptions dispensed. [..] From 2009 to 2018, the percentage of employer-sponsored plans using high cost-sharing drug tiers (fourth or specialty tiers) rose from 11% to 51%, and the disparity in out-of-pocket spending between specialty-drug users and nonspecialty-drug users also increased, becoming 3 times as large as that in an earlier 10-year period. This spending increase imposes substantial financial burdens on a small population of patients who already bear a serious disease burden.
[..] We constructed a data set at the patient-month level using administrative claims data from Aetna, Humana, and UnitedHealthcare commercial plans provided by the Health Care Cost Institute. The data contained information on enrollment, demographic characteristics, health-plan characteristics, pharmaceutical and medical utilization, and costs for more than 50 million members per year. We linked members’ five-digit ZIP Codes to area-level socioeconomic status using data from the 2015 American Community Survey.
[..] Persons were required to have two or more outpatient medical claims (on separate dates) with diagnoses for the same disease of interest or one or more inpatient or emergency department claims with diagnoses for diseases of interest: rheumatoid arthritis, multiple sclerosis, hepatitis C, psoriasis, psoriatic arthritis, Crohn’s disease, or ulcerative colitis [..]. We excluded persons who had two claims with cancer ICD codes (except codes for nonmelanoma skin cancer) to avoid including orally administered anticancer treatments that were subject to oncology parity laws over the same period, since we could not distinguish between the effects of specialty drug caps and oncology parity laws for these drugs.
[..] For specialty-drug users in the 95th percentile of specialty-drug out-of-pocket spending overall (evaluating all three intervention states [DE, LA, MD] and years together), caps were associated with a change in specialty-drug out-of-pocket spending of −$351 (95% confidence interval [CI], −554 to −148) per user per month, representing a 32% reduction in spending. [..] In contrast, caps were not associated with changes in other out-of-pocket spending outcomes, health-plan spending outcomes, or specialty-drug utilization outcomes, with the exception of an increase in the utilization of specialty drugs in Delaware (mean increase, 3 days’ supply [95% CI, 1 to 4]) and in the third postpolicy year (mean increase, 3 days’ supply [95% CI, 1 to 5]).
[..] We found that among patients with the highest levels of specialty-drug spending, state legislation capping out-of-pocket costs at $150 per 30-day specialty-drug prescription was associated with a reduction of $351 per person per month in out-of-pocket spending. [..] Exploratory analyses revealed a larger change in spending for persons with a diagnosis of hepatitis C than for persons with other diseases of interest, which suggests that the policies may be more effective at protecting against very high out-of-pocket prices incurred over a shorter duration.
Our results suggest that the policies may be well aligned with health economic principles for insurance coverage. Insurance functions best when it provides coverage for treatments that are high-cost, that are for rare conditions, and that patients value (e.g., treatments for which changes in out-of-pocket prices do not substantially alter utilization behavior). Aside from being used to treat relatively rare conditions and being expensive, specialty drugs may be good candidates for generous coverage because they tend to be clinically important medicines, and previous research has shown limited price sensitivity for specialty drugs, given their clinical importance and lack of appropriate substitutes. Some treatments, such as those for hepatitis C, are curative therapies with minimal side effects. Other treatments, such as those for multiple sclerosis, rheumatoid arthritis, or Crohn’s disease, substantially improve quality of life and activities of daily living and have few viable alternatives.
[..] Since a primary function of insurance is to spread the financial risk of catastrophically high spending for a small population, we interpret the caps as strengthening this risk-spreading function without detectably increasing spending for the broader population.”
Patient and Plan Spending after State Specialty-Drug Out-of-Pocket Spending Caps, Yeung K, Barthold D, Dusetzina SB and Basu A. NEJM 2020.8.6
2020.8.4
“In 2016, life expectancy of American women (81.4 years) was 3.0 years below the female average of high‐income countries and 5.8 years below the leader; life expectancy of American men (76.4 years) was 3.4 years below the male average and 5.2 years below the leader. The fall of the United States to the bottom in international rankings began in the 1980s, first with slower gains in longevity than other countries and then with absolute declines in recent years. Among 22 high‐income countries, the United States fell from thirteenth place in 1980 to the bottom by the early 2000s.
[..] In 2013, a report commissioned by the National Research Council outlined five potential explanations: public health and medical care systems, individual behaviors, social and economic factors, physical and social environments, and policies and social values. Studies to date have largely focused on the first three explanations, with mixed evidence about their contribution. Some researchers assert that medical care could contribute only a small extent to the US longevity disadvantage, noting that the disadvantage exists even among Americans with health insurance; the United States spends more on medical care than any other country; shortfalls in medical care explain just 10%‐15% of preventable mortality in the United States; and deaths from external causes (suicides, homicides, accidents), which increasingly comprise a sizable part of the disadvantage, are not determined by medical care. Other studies note that Americans engage in some unhealthy behaviors more so than do individuals in peer countries. For example, Americans have the highest average caloric consumption in the world and have historically had higher smoking rates than peer countries. However, even a highly risky behavior like smoking cannot explain why the US mortality disadvantage is pronounced below age 50. Socioeconomic factors might also contribute to the US disadvantage, particularly given the relatively high prevalence of poverty and income inequality. Yet, even highly educated and high‐income Americans (particularly women) have worse health and shorter lives than their peers in many other high‐income countries. Importantly, even if proximal explanations such as smoking, diet, poverty, and medical care did explain the disadvantage, they do not explain why Americans used to smoked more, consume more calories, experience higher poverty levels, are less likely to have health insurance, and so on. Doing so requires examining upstream factors and taking a political economy perspective.
[..] there is compelling evidence that the falling position of the United States in international rankings of life expectancy in the post‐1980 era partly reflects the growing geographic disparities in health and longevity within the United States. For instance, after examining life expectancy at age 50 in the United States and other high‐income countries (Canada, France, Germany, Japan) between 1980 and 2000, Wilmoth and colleagues concluded that 10% to 50% of the growing life‐expectancy gap between the United States and those countries was attributable to growing geographic variation within the United States, alongside shrinking variation in the other countries, with the growing US variation being the driving force.”
The researchers estimated state life expectancy by state using the United States Mortality Database. The group reviewed 135 state policies across 18 domains:
- Abortion
- Campaign finance
- Civil rights and liberties
- Criminal justice
- Education
- Environment
- Gun control
- Health and welfare
- Housing and transportation
- Immigration
- Private sector labor
- Public sector labor
- LGBT rights
- Marijuana
- Taxes
- Voting
- State excise taxes on tobacco
- Overally policymaking activity
“Liberal was defined as expanding state power for economic regulation and redistribution or for protecting marginalized groups, or restricting state power for punishing deviant social behavior; conservative was defined as the opposite.
[..] If all states’ policies had the maximum liberal score on the policy measures, the model estimates that US life expectancy would be 2.8 years longer among women and 2.1 years longer among men. If all states’ policies were the same as Connecticut in 2014 (Connecticut made the largest shift toward liberal policies between 1970 and 2014), we estimate that US life expectancy would be 2.0 and 1.3 years longer among women and men, respectively. However, if those policies imitated Oklahoma in 2014 (Oklahoma made the largest shift toward conservative policies), US life expectancy would be an estimated 1.0 and 0.5 years shorter among women and men, respectively. In addition, the model estimates that the status quo—allowing the current policy direction of the states to continue—would yield minimal improvement in longevity: US life expectancy would be 0.4 and 0.3 years higher among women and men, respectively.
[..] We found that policies on tobacco, labor, immigration, civil rights, and the environment were strongly associated with longevity among women and men, with more liberal versions of each policy within a state predicting a nearly 1‐year increase in that state’s life expectancy. [..] more liberal policies on abortion and gun control predicted longer life expectancy among women, while more conservative marijuana policies predicted longer lives for both women and men. A review of the effect of marijuana policies on outcomes such as usage and marijuana‐involved emergency room episodes reported both null and negative effects, and suggested that the evidence was inconclusive given the difficulty in measuring the heterogeneity in marijuana policies. Taking these findings together, the slow gains in US longevity may partly reflect the national shift toward some conservative policies that are negatively associated with longevity (eg, abortion restrictions, reductions in gun control) offsetting the national shift toward some liberal policies that are positively associated with longevity (eg, environment and civil rights protections).
[..] the analyses do not prove that state policies have a causal effect on life expectancy. Our analyses were intended to estimate changes in life expectancy within a state from changes in a large set of policies within a state, without making definitive causal claims.
[..] The high‐profile annual reports on life expectancy from the US Centers for Disease Control and Prevention focus on national trends and can give a false sense of stability. Even the recent reports of declining US life expectancy mask more dramatic declines occurring at the state level. We recommend that national health reports prominently feature information by state. We also recommend that large‐scale efforts to track US health and longevity, as well as international comparisons in scientific research, include data on US states.”
US State Policies, Politics, and Life Expectancy, Montez JK, Beckfield J, Cooney JK et al. Milbank Quarterly 2020.8.4
2020.7.31
“Several years ago, the Digital Bridge collaborative was formed. It consists of representatives of the three key stakeholder communities in this crucial arena: public health, the health care delivery system, and electronic health record (EHR) vendors. They concluded that the ubiquitous footprint of electronic health records in the United States should be the standard source of rich, real-time data for public health purposes and was equally ideal as a set of recipient systems for critical public health guidance for clinicians and patients. What did they all stand to gain from participation? Public health stakeholders could get automated, standard, complete, and near real-time data flows for surveillance and registry purposes. Health care stakeholders could fulfill their reporting obligations accurately and completely, at much lower cost, and without disrupting the workflows of physicians and nursing staff. The EHR vendors would be able to meet their clients’ reporting requirements in a single, standardized way, independent of reporting jurisdiction.
[..] When it was decided that electronic case reporting (eCR) for surveillance purposes was to be the first use case, the HL7 electronic initial case report (eICR) and reportability response standards were chosen; it was decided that two existing software platforms, the Association of Public Health Laboratories Information Management System (AIMS) and the Reportable Conditions Knowledge Management System (RCKMS), would form the core of the system. AIMS is developed and maintained by the Association of Public Health Laboratories in cooperation with the Centers for Disease Control and Prevention (CDC). It performs the data validation, extraction, service hosting, response creation, routing, and transport function. RCKMS is developed and maintained by the Council of State and Territorial Epidemiologists (CSTE), also in cooperation with the CDC. It provides the codes (SNOMED CT, ICD-10, and LOINC) that would trigger an eICR and runs a decision support service using jurisdictional reporting rules to determine reportability and where the report should be routed.
The flow goes like this: The CSTE determines all of the diagnosis and laboratory test and result codes of interest for public health efforts as triggers for an eICR. These codes are distributed via the electronic reporting and surveillance distribution service from AIMS, and the standard EHR platforms import, or “consume” the codes and imbed them as triggers for identifying reports to be created and sent. This consumption occurs on a regular basis and is also executable urgently.
If a clinician, in the course of documenting care in an EHR, uses an expression that generates one or more of the published codes, then an eICR is automatically generated and transmitted via the AIMS platform for processing by RCKMS, where the jurisdictional reporting rules operate on the eICR and if determined reportable, transmit it to the appropriate public health agency or agencies. An automated response is returned to the sending EHR to share the reportability determination and provide additional information about that condition and other references and be filed in the patient record. This response could be refined in the future to request more data from the EHR and the clinicians caring for the patient, and it can transmit guidance for the care of that patient directly to the inbox of the clinician of record.
[..] At the end of January 2020, CSTE identified the trigger codes for COVID-19 infection, the EHR vendors from the initial sites consumed the new COVID-19 codes into their production software, and COVID-19 case reports began flowing from those initial sites to the correct health departments literally overnight.
[..] From the initial four delivery system sites, more than 2,400 facilities from 26 systems are now transmitting these reports, with more being added weekly. A Fast Healthcare Interoperability Resource eCR Now app directed at smoothing adoption by a delivery system has been developed, tested, and deployed. If a delivery system is already using eCR-enabled EHR software, the process of onboarding typically takes only three to four business days.
What are the limiting factors? First, although all state health departments can now receive eCR messages, many of them cannot handle those messages in an automated way. Their disease surveillance systems vary widely in their capabilities. Second, many health departments do not have the information technology resources to analyze the surveillance data once they have it nor is it easy for them to retransmit that data to the CDC.
[..] If the business-as-usual approach to the disbursement and use of these funds is allowed to persist, we could essentially have 50 proprietary solutions to the solitary problem of developing accurate surveillance for COVID-19 cases, and there would be as many ways of transmitting that data to the CDC. States would have preserved autonomy, but the country would likely endure heterogeneous, noninteroperable systems that would undermine rapid understanding of local, regional, and national trends regarding COVID-19 or any other reportable condition.”
A Digital Bridge To Real-Time COVID-19 Data, Lumpkin JR and Wiesenthal A. Health Affairs blog. 2020.7.31
“The origins of vaccine hesitancy—recognised by WHO in 2019 as one of the top ten threats to global health—reach back to compulsory smallpox vaccination laws and the thread of this long history continues today.
[..] Heidi Larson’s compelling new book Stuck: How Vaccine Rumors Start—and Why They Don’t Go Away looks at the dynamics of the evolving debate through the lens of an anthropologist who has been studying vaccine confidence for decades.
[..] The foundation that underpins vaccination acceptance is trust. Trust in the processes, practices, and policies of vaccine development, licensure, and manufacturing; in the policy makers who set vaccine recommendations; and in the health-care system—the doctors, nurses, and community immunisers who administer vaccines as part of routine care and during mass vaccination campaigns. Without understanding and addressing trust, efforts to improve vaccine confidence will be a steep climb. That will certainly be the case when COVID-19 vaccines arrive, especially given the many new vaccine technologies that are being tested and the speed at which they are being developed.
[..] The calculus of vaccination decision making is the balance of benefit and risk coupled with uncertainty and Larson argues that it is these same elements that breed rumours. Because no vaccine—and no medical product— is risk free there will always be fertile ground for rumours. The challenge, Larson stresses, is “managing the rumours and mitigating purposeful scare tactics while listening for important clues that need further investigation”. These are not moles to be whacked, but signals that call for a deeper understanding not only about why they came about but why they stick. Only by doing this are we likely to get unstuck.
Despite tremendous gains that have resulted from making vaccines more accessible and affordable and the delivery programmes that make them available, as Larson highlights in this book there has been stagnation of vaccine uptake. Although vaccination remains the social norm in all countries, this plateau in uptake together with outbreaks of vaccine-preventable diseases has led to a sharper focus on the quality of vaccination services and on the last inch of the last mile: the decision to accept or decline a vaccine that is available and being offered.
[..] But Larson asks that we do more because it isn’t only about getting the facts right. As she frames the core problem: “we don’t have a misinformation problem, we have a relationship problem”. The misinformation can be deleted, but the underlying distrust that has caused it and allowed it to stick remains. Rather than countering and dismissing rumours, Larson encourages the health community and other stakeholders to listen to these rumours and recognise what people are saying. These analyses can reveal deeper issues such as the feeling of being disenfranchised and not being heard. It is from these insights, she argues, “lie the cues to building new and more trusting relationships”.
[..] there is a need to address the complex challenges related to vaccine hesitancy that Larson’s book illuminates. She captures in a single sentence the crux of the issue: “Today we are in the paradoxical situation of having better vaccine science and more vaccine safety regulations and processes than ever before, but a doubting public.” To avoid getting stuck before COVID-19 vaccines become available, concerted efforts by health and other sectors, governments, and civil society will be needed to explain what we know and don’t know about the vaccines that have been approved for widespread use, their benefits and risks, and the value to individuals and communities that make the case for vaccination. It will be crucial that such efforts listen to, involve, and engage all communities at the local level.”
Why vaccine rumours stick—and getting them unstuck, Gellin B. Lancet 2020.8.1
2020.7.30
“The Medicaid program was designed to improve public health by providing coverage for essential health services to low-income populations. The Social Security Amendments of 1965 prohibited the use of federal funds for medical care provided to “an inmate of a public institution.”(p71) Decades later, this policy, known as the Medicaid Inmate Exclusion Policy, still prohibits Medicaid from financing care while individuals are incarcerated. However, the services that Medicaid covers could serve as a model for a reasonable set of mandated health services within correctional facilities to ensure care in these institutions is commensurate with care available in the community. We propose mandating that correctional facilities provide access to all health care services covered by Medicaid in the community through legislation by federal, state, and local authorities that oversee health care provided in correctional facilities within their respective jurisdictions. Such mandates would provide uniform standards across local, state, and federal correctional facilities, fulfill Eighth Amendment rights, improve continuity of care for individuals receiving Medicaid-funded care prior to incarceration, and facilitate smooth transitions at release.
[..] Although expanding benefits for persons who are incarcerated has historically lacked political support, the exponential growth of incarceration because of structural racism, coupled with the vulnerabilities revealed by the COVID-19 pandemic, have made it clear that health care provided inside jails and prisons is essential to reducing inequities and improving the public’s health.
[..] Mandating essential health services that are comparable with those covered by Medicaid can ensure the fulfillment of constitutional requirements to provide care to people who are incarcerated and encourage better oversight from local and state health authorities. Improving health care in correctional facilities can help to address numerous public health crises associated with infectious disease, substance use, chronic disease, and mental health among some of the nation’s most vulnerable populations. The COVID-19 pandemic requires a reexamination of correctional health care to ensure jails and prisons provide uniform care comparable with community standards. Most people who are incarcerated return to the community. It is in our nation’s best interest to promote their health and success.”
Aligning Correctional Health Standards With Medicaid-Covered Benefits, Olson MG, Khatri UG and Winkelman TNA. JAMA Health Forum 2020.7.27
“How well can virtual care replace physical care? What are the risks?
Lessons may be learned from the prior experience of the UK National Health Service (NHS) with Babylon Health. Babylon, a health care start-up, launched its service in fall 2017. Using a small primary care practice in West London as a point of entry, Babylon flooded Facebook, bus stops, and the subway with advertisements promising free, 24/7, virtual-first primary care and rapidly expanded to serve nearly 60 000 patients across London and Birmingham. A high-profile, technology start-up entered a market where there was no advertising (and no “poaching” of patients from other practices) and a long history of clunky and failing health information technology.[..] By offering video and telephone appointments, it also disrupted the traditional geographic link between primary care practices and patients. Thanks to an independent evaluation, the NHS experience with Babylon Health also generated evidence on who used it and for what.
[..] Who used Babylon Health? Compared with the average NHS practice, patients were younger (94% were younger than 45 years), relatively healthy (only 10% had 1 of 5 major long-term conditions, which was less than the age-adjusted London average), wealthier, and more educated (more than 80% were educated to at least college level). This pattern was arguably by design; the NHS restricted patients with chronic medical conditions and those who were pregnant from signing up, citing safety concerns about these groups using a model based primarily on virtual consultations. But it also largely reflects what we already know about digital health care—that there are disparities in engagement driven by ethnicity, age, and socioeconomic status and that these disparities can lead to widening health inequalities.
[..] The evaluation of Babylon Health showed that patient experience was largely very positive, even for those with long-term conditions (though less so for those with particularly complex needs), and patients felt that Babylon Health offered higher-quality care than their previous practice. However, the rate of turnover was high (around a quarter of patients deregistered), with some suggestion this was driven by changing health needs and a desire to be able to directly book a face-to-face appointment. It may be that virtual-first care was inappropriate or inconvenient for certain conditions.
Evidence from other countries, notably Sweden, on what patients consulted for may shed light on this issue (Babylon did not share data on this, citing commercial confidentiality). This showed that the most common condition among women was urinary tract infection, and among men, it was upper respiratory infection. In the US, prior to the COVID-19 pandemic, telehealth was primarily used for psychiatry and urgent care. Now, with almost all care moving online, the number of conditions treated with telehealth has widened. For some, it will work well; for some, it will be simply adequate but worth the trade-off with the risks of in-person visits; for others, it will be ineffective or possibly dangerous. Discerning which conditions fall into which category will be essential to building an effective, safe, post–COVID-19 telehealth world. To accomplish this goal, health systems will need to ensure that they are collecting the data on who is using their telehealth services, for what reasons, and—to the extent possible—what their quality of care and outcomes are. When contracting with virtual care providers, insurers need to ensure that they, unlike the NHS in Babylon Health’s case, can access the data collected. Analysis of these data can wait, but data collection cannot.”
Virtual Primary Care—Is Its Expansion Due to COVID-19 All Upside? Krelle H, Dodson JA and Horwitz LH. JAMA Health Forum 2020.7.29
“Medicare-for-all proposals advanced by such politicians as Sen Bernie Sanders (I, Vermont) and Sen Elizabeth Warren (D, Massachusetts) have encountered skepticism from many liberals, as well as heavy criticism from conservatives.
One objection is the enormous increase in federal expenditure that would be involved in such a switch, and although supporters point to the large savings in private expenditures, the net costs depend on many considerations and design features.
Another concern, applying to some versions of Medicare for all, is that although the Medicare benefit package is comprehensive, traditional Medicare has significant out-of-pocket costs for all but the lowest income beneficiaries (who qualify as “duals” for overlapping Medicaid coverage). This feature effectively requires seniors to purchase private “Medigap” coverage as a supplement.
A third concern is disruption. This is the other side of the coin associated with having multiple health systems in the US; Medicare for all would mean big changes for most individuals with existing coverage.
[..] Unlike the higher-profile Medicare-for-all approach, a Medicare Advantage–for-all approach would have several advantages. For instance:
- Medicare Advantage has wide popular support as well as broad political support. Medicare Advantage enrollment has been growing rapidly, doubling in the last decade, with the proportion of Medicare beneficiaries in such plans now exceeding 34% and rising. Moreover, Republicans as well as Democrats have supported and expanded Medicare Advantage, and the idea of making Medicare Advantage plans available to younger US residents has begun to intrigue some reformers on the right.
- The capitation system permits competing Medicare Advantage plans to offer a variety of benefits beyond a required core of basic benefits. Moreover, in contrast to traditional Medicare’s rigid and detailed payments system, it allows plans to explore different payments as a means of achieving greater efficiency and beneficiary satisfaction.
- In contrast with the design of traditional Medicare, Medicare Advantage plans are generally consistent with the growing managed care pattern in nonelderly coverage, including within the employer-based system. Today, about 90% of Medicaid beneficiaries are enrolled in some form of managed care. Meanwhile, about two-thirds of workers with employment-based plans are enrolled in health maintenance organizations or other network coverage that is similar to most Medicare Advantage plans. Medicare’s income-adjusted premiums are also broadly compatible with the structure of income-based subsidies available for plans in state health insurance exchanges, and many insurers offer Medicare Advantage and health insurance exchange plans that have similar designs. Thus, for a large proportion of households, transitioning from their existing coverage to coverage more like Medicare Advantage plans would not involve a big adjustment.
- Recent changes in laws and regulations allow Medicare Advantage plans to include more nonclinical services that can influence health, such as nonurgent transportation, nutritional services, and even some simple home modifications to reduce the risk of injuries. This reflects the growing interest in addressing so-called social determinants of health.
[..] Choosing Medicare Advantage as the organizing theme for reforming the whole US system does not necessarily imply there must be radical legislation that literally replaces all existing coverage with the current Medicare Advantage program. That would be unnecessarily disruptive and regimented. Rather, it should mean gradually adapting existing forms of coverage so that over time they become very similar to Medicare Advantage, and there would essentially be no change in coverage as individuals change jobs, lose their jobs, or retire.
One step toward that outcome would be to merge state exchange plans with Medicare Advantage plans in the state. Another would be to slowly reconcile the subsidy system available for exchange plans with the tax benefits for employer-sponsored insurance, such that a similar structure of income-related subsidies would apply to everyone enrolling in insurance. Seniors would continue to receive assistance toward the cost of coverage that is reflective of the payroll taxes they paid and the national commitment to their health care, at least until there was agreement on a more comprehensive revenue and financing system, and the state-federal share of support would continue for lower-income households. A third step would be to move further toward the place of work being just a convenient location to facilitate plan selection, with employers handling the mechanics of government subsidies and payments by workers, and to move away from employers as plan sponsors.”
Medicare Advantage for All, Perhaps? Butler SM. JAMA Health Forum 2020.7.30
“Developments over the past twenty years have not altered the fundamental improvement aims and health system redesign recommendations identified in Crossing the Quality Chasm. [..]
Perhaps the most significant lesson was the impact of standardized data. Across the financial and transportation sectors, standardized data and financial reporting processes have provided important consumer safeguards and enabled valid, transparent, and benchmarked metrics to reliably compare information across companies. For example, key financial health terms and underlying data—such as earnings per share (EPS) and earnings before interest, taxes, depreciation, and amortization (EBITDA)—are universally defined and audited for validity. Audited financial statements based on standardized terms and data can be easily accessed from the Securities and Exchange Commission and used for a variety of purposes.
By comparison, in the health care sector, multiple definitions may exist for critical terms and measures, undermining peer-comparisons and data analyses. Furthermore, the relevant data may not be readily available. An organization’s accounting system is the hub of financial data, but a unified repository with complete patient data does not exist for health care; data is typically captured in discrete environments with limited interoperability. Electronic Health Records (EHR) are increasingly viewed as the hub of health care data; however, they face challenges in unifying patient data across an increasing number of sources.
The lack of standardized data in health care undermines the free flow of data into, out of, and among silos. This challenge becomes more acute as the number of relevant data sources grows (e.g., condition-specific registries) and as new partners enter the ecosystem (e.g. Community Benefit Organizations that are capturing critical information related to social determinants of health).
[..] We outline below five strategic objectives that represent critical priorities for policy development and action.
- Implement seamless flow of reliable data
- Ensure appropriate, safe, accessible care
- Pay for person-centered care and healthy communities
- Support activated consumers, and
- Achieve actionable transparency”
High-Value Care Every Time: Recommendations From The National Quality Task Force, D’Avena A, Agrawal S and Kizer K. Health Affairs blog 2020.7.30
“After 2 decades of efforts relying largely on quality measurement and performance-linked payment incentives, we need new ideas and new conversations. As revealed by health care workers’ response to the Covid-19 pandemic, professionalism in health care may be an underused resource.
[..] A central concept in health economics is that the physician acts as an agent for the patient, determining what the patient’s problem is and what should be done about it. While patients desire high-quality care, they may not be sufficiently informed to demand it. Physicians are more informed than patients by virtue of their training and experience, and are expected to be motivated by their intrinsic concern to use that knowledge in their patients’ interest. Professionalism can be thought of as determining the outcome of physician agency (how patient welfare is served by physicians’ knowledge and concern). Conceptually, with informed and motivated professionals as their agents, patients effectively become discerning consumers capable of driving healthy competition in health care markets where extrinsic pressure may be needed to encourage high-quality care (e.g., primary care physicians [PCPs] directing patients to the safest hospitals or surgeons selecting the best devices).
[..] Early data indicating that physicians are not perfect agents with perfect information spurred the growth of quality measurement, which has uncovered more such evidence. Empirical observations that physicians can be misinformed, unaware of evidence, subject to biases, and influenced by financial incentives upended physicians’ long-standing position as unquestioned and self-regulated authorities. With these shortcomings exposed, consensus emerged that physicians could no longer be solely entrusted to know and do what is best for their patients.
[..] Without linked payment incentives, measures may be used privately for quality improvement initiatives or publicly to inform consumers and providers in a market. In recent years, we have focused almost exclusively on the box of strategies that combine measurement with payment to make up for weak competition or deficient provider agency by tying financial incentives directly to performance on specific measures. At best, the gains have been spotty and perhaps not surprisingly so. Measure-reliant strategies such as public reporting, pay for performance, or value-based purchasing are constrained by the multidimensional nature of quality and the challenges inherent in measuring and rewarding it.
First, focusing on measurable markers of quality can divert resources from harder-to-measure but equally or more important aspects of care, resulting in unchanged or even worse quality overall. [..] Second, performance measures detect the symptoms of dysfunction, not necessarily the cause. Thus, performance-linked incentives often elicit low-cost responses that improve measured performance (e.g., teaching to the test or gaming) but do not address the underlying disorder. [..] Third, risk adjustment presents a thorny challenge with no satisfying solution, particularly for outcome measures such as functional status or mortality. When adjustment is incomplete (as it will always be to some extent), budget-neutral pay-for-performance programs transfer resources between providers partly based on the patients they serve rather than the care they deliver. [..]
Fourth, whereas payers can set strong incentives for providers to minimize costs without having to measure provider costs (e.g., via capitation contracts), financial incentives to improve quality as a whole are inherently weaker because quality must first be measured to serve as a basis for payment. As an enormously complex construct, quality cannot be measured in its entirety. The bulk of reimbursement will always be unrelated to quality. Paying on numerous measures further weakens incentives to improve on any one dimension, whereas paying on fewer may support stronger incentives for meaningful change but only for a narrow slice of quality.
Turning to experience to date, gains from performance-linked payments have generally ranged from absent to modest and have come at great expense — including substantial reporting costs, the deadweight loss from wasteful score-promoting behaviors, and an inequitable and potentially harmful redistribution of resources. Harder to quantify, but no less real, are the insidious effects that performance-based pay have on professionalism. As the concept of quality is reduced to that which is measured, improvement redefined as higher scores, extrinsic judgments elevated above unseen efforts, and time for patients and colleagues hijacked by box-checking, demoralization sets in. Purpose is undermined as demands on physicians diverge from their values, professional identity is lost, and intrinsic motivation gives way to a self-fulfilling prophecy that physicians care only about financial incentives.
[..] Recognizing the costs, experts agree that the deployment of quality measures needs to be rethought. Yet in the scramble for new directions, the conversation is still dominated by a measure-reliant orientation. Measure enthusiasts offer only incremental suggestions — such as introducing more “skin in the game,” limiting the number of measures, and improving risk adjustment — or inviable aspirations to link strong incentives with fanciful measures that somehow capture all that we care about and are immune to the problems above.
[..] W. Edwards Deming — a leader in the field of quality improvement — incisively noted: “It is wrong to suppose that if you can’t measure it, you can’t manage it—a costly myth.” Moreover, reliance on scorecards and pay for performance is at odds with the basic economics of market functioning. Economic theory points out that quality improvement does not require quality to be converted into a contractible or manageable quantity. Quality just has to be observable to whoever is motivated to benefit from it.”
Dr. McWilliams suggests a series of ideas (e.g., allowing primary care providers to judge specialist performance based on consultation quality and patient feedback, use physician perceptions of one another to identify sources of best practices) but admits most have not been studied in any detail.
“Thus, incentives at an organizational level that promote — or at least do not interfere with — physicians’ intrinsic motivation are important. The goodwill and professionalism of physicians need not be “bought with tips,” as health economist Uwe Reinhardt once noted, but it can be exploited by organizations to serve financial interests not shared by physicians or patients. Beyond changes in payment systems, there are mechanisms by which informed and motivated physicians might influence organizational agendas. If professionalism can be directed to shape organizational objectives and capabilities, the benefits may not be as limited as they may seem.
[..] organizations compete not just for patients, but for clinicians, too. Indeed, the physician labor market could become an engine of long-awaited gains. [..] There is reason to believe that physicians recognize organizational quality and exhibit quality-related preferences in choosing a workplace. For example, physician perceptions of greater clinic capacity to address patient needs have been associated with lower rates of burnout. Likewise, opportunities to spend more time with patients and shed reporting and documentation requirements have been cited as primary motivations for PCPs leaving practices in favor of direct primary care models.
[..] Yet physicians have limited options in consolidated markets and are constrained by high switching costs. Steps to improve physician mobility might include: limiting noncompete clauses that restrict where physicians can work and limit their ability to take patients with them after leaving an organization; greater EHR interoperability so patients can follow their physicians; team-based models that minimize the costs of rebuilding patient panels and learning new systems; and simplified licensing and credentialing processes. There are also opportunities for better informing choices. Physicians cannot readily access anonymous testimonies about their job options from current or former practice members; the market for physician recruitment services seems ripe for disruption. With such pieces in place, physicians might be more likely to leave organizations if they detect poor quality, and organizations might be more likely to recruit and retain physicians by demonstrating capacity to deliver high-quality care.
[..] Because physicians hold themselves and others to high standards and value their reputation, peer comparisons and peer accountability have been advanced as particularly effective motivators. The provision of information on comparative performance alone may strengthen intrinsic incentives to improve and might explain any gains derived from public reporting. The application of these principles, however, has generally been limited to performance measures targeting specific actions, such as appropriate medication prescribing. Broader nudges could cultivate broader improvement.
For example, clinicians’ case notes could be randomly sampled for weekly peer discussions moderated by peer-elected master clinicians, with preference for cases with high-risk patients, adverse outcomes (e.g., hospitalization following a visit), or complex decision-making (e.g., a high number of tests, studies, and referrals). Similarly, surgical procedures could be recorded and sampled for review among colleagues. [..] When observed by well-trained eyes, providers may be particularly inspired to elevate their game. The incorporation of peer accountability and feedback additionally leverages the importance to physicians of local reputation and should encourage critical and evidence-based thinking that survives group scrutiny. Other strategies for better positioning clinicians to learn from peers, including team-based models and searchable records, should similarly contribute to this dynamic. We can do much more than infrequent morbidity and mortality conferences or costly external coaching sessions. Peer-to-peer teaching and learning that is constructive and collegial can be integrated into practice routines. Such forums are not foreign to physicians; indeed, a supervisory version serves as the basis for residency training yet all but vanishes thereafter.
[..] Physicians will never be perfect agents. Regulatory safeguards, managerial accountability, and complementary strategies are needed. Data-driven remediation of human error and private use of measures for internal monitoring will continue to play roles. Leadership will matter. But as we learned from the Covid-19 response, immeasurable good can come from physicians’ motivation to learn and do what is best for their patients.
[..] A lingering question is how the development and adoption of successful new strategies will be encouraged if not contractible through the payment system. Although unsatisfying to regulators, ultimately the spread of better care — once identified — will rely to a large extent on patients wanting to receive it and clinicians wanting to deliver it. Competition and other mechanisms can strengthen responsiveness to those demands. Removal of distracting incentives will be key. But improvement might require a change in emphasis from interventions conceived to score movement on a specific measure to those conceived to support the elements of high-quality care and evaluated using a broad range of measures, including clinician views: a paradigm shift from seeking successful measures to seeking measurable success.”
Professionalism Revealed: Rethinking Quality Improvement in the Wake of a Pandemic, McWilliams JM. NEJM Catalyst 2020.7.22
[Click here for earlier content]